Unit 5: Telemedicine Services
2.5 Introduction to Telemedicine
2.5 Prescribing Protocol for Telemedicine Services
2.5 Services Provided by Well360 Virtual Health and Approved Telemedicine Vendors
2.5 Virtual Outpatient Office Visits
2.5 Outpatient Virtual Mental Health/Substance Abuse (Substance Use Disorder)
Many factors can make it difficult for patients to get appropriate medical care when they need it — geography, weather, availability of specialists, transportation, and others. With advancements in technology that allow for communications and information exchange at a distance, the telemedicine field is evolving rapidly to meet the needs of the patient community.
Telemedicine includes a growing variety of applications and services using two-way forms of telecommunications technology. The use of this technology is now becoming integrated into the ongoing operations of hospitals, specialty departments, and physician offices. For both providers and patients, telemedicine can play a significant role in facing the challenges of maintaining or improving health care outcomes while reducing costs.
Some of the most important benefits of telemedicine include accessibility and flexibility for the patient community. With the mounting shortage of physicians, especially for primary care, telemedicine offers patients the convenience of connecting with medical professionals more easily when traveling, pressed for time, unable to take time off from work or school, or not able to drive long distances to see their health care provider.
What is Telemedicine?
Telemedicine is defined as the exchange of medical information between sites via electronic communication for transmitting clinical information for diagnostic, monitoring, and therapeutic purposes. The term “telehealth” is often used in conjunction with telemedicine and is intended to include a broader range of services using telecommunication technologies, including videoconferencing. These terms are often used interchangeably.
Telemedicine is revolutionizing health care by bringing medical services directly to patients, regardless of their location. It utilizes technology like video conferencing, mobile apps, and remote monitoring devices to connect patients with health care providers. This allows for a wide range of services, from virtual consultations and diagnosis to remote monitoring and even surgery.
Highmark is committed to expanding access to quality care for our members and providing new options for more timely and convenient access to meet their needs. In our efforts to expand services and coverage to more members, we are providing telemedicine coverage options through:
- Well360 Virtual Health offers services provided by our approved telemedicine vendors via real-time interactive audio and video telecommunications technology. These vendors provide access to a national network of board-certified physicians.
- Benefit enhancements that provide coverage for “virtual visits” with our members’ trusted network providers using telecommunications technology.
- Telemedicine can be delivered via a real-time 2-way audio-only conversation in Delaware (DE), New York (NY), Pennsylvania (PA), and West Virginia (WV) – but in DE and NY, 2-way audio is limited to when the patient must be unable to access the appropriate broadband service or other technology necessary to establish an audio and visual connection.
- *Note: Highmark Medicare Advantage plans continue to follow the Centers for Medicaid and Medicare Services (CMS) guidelines for telemedicine visit coverage and reimbursement. Only the codes identified by CMS as appropriate for telemedicine services will be reimbursed by Highmark for Medicare Advantage members.
Highmark expects contracted providers to render telemedicine services in compliance with applicable laws and regulations. Providers who have questions about laws applicable to the practice of telehealth and telemedicine should consult with their attorney to ensure they are compliant with requirements appliable to their practice.
Reimbursement Policy 046
For information on billing and reimbursement for commercial and Medicare Advantage products, please see:
Highmark Reimbursement Policy RP-046: Telemedicine and Telehealth Services.
This policy includes complete guidelines for both professional and facility billing requirements for reimbursement, including the use of Place of Service code 02 or code 10 on all professional telehealth claims and the modifiers needed for both professional and facility claims.
Reimbursement policies are available on the Provider Resource Center under Claims & Authorization, then Reimbursement Programs, and choose Reimbursement Policies.
The standard of care applicable to an in-person patient encounter also applies to a virtual patient encounter. Telemedicine consultations and treatment, including the authorization and dispensing of prescription medication(s), must be held to the same professional standards of appropriate medical practice as traditional in- person patient encounters.
Prior to issuing prescriptions via telemedicine, providers must ensure that a provider-patient relationship is established and documented in the member's file. A proper “provider-patient relationship” may be established when the provider (physician/practitioner) obtains all relevant medical history and conducts an appropriate evaluation to establish a diagnosis(es) and identify underlying conditions or contraindications to recommended treatment.
A valid provider-patient relationship may be established using telemedicine technologies provided the appropriate standard of care is met and all applicable state and federal statutes and regulations are followed. The services to establish the provider-patient relationship during the initial encounter, as described above, must take place via an interactive audio and video telecommunications system (unless exceptions are allowed for certain medical services as appropriate under applicable state laws).
Providers should give careful consideration in determining whether an in-person office visit for the initial visit would be beneficial in establishing a provider-patient relationship based on the member’s presenting condition(s). While some situations are appropriate for using telemedicine technologies for member care in lieu of the traditional in-person office visit, others are not.
Methods That Are Not Acceptable
A provider-patient relationship may not be established through, but not limited to, the following:
- Internet questionnaires;
- Social media;
- Email messages;
- Patient-generated medical history;
- Text messages;
- Facsimile (fax) machine; or
- Any combination of the above.
These do not constitute acceptable standard of care and prescriptions cannot be issued to Highmark members when a provider seeks to establish a provider-patient relationship with the member based solely on these methods.
The following guidelines apply when using telemedicine technology to issue prescriptions to Highmark members:
- Prior to issuing a prescription, all relevant information that shows that a provider-patient relationship has been established (e.g., patient demographic information, chief complaint, history of present illness, allergies, medications, past medical and surgical history, family and social history, etc.) must be documented and maintained in the member’s medical record as required with in-person diagnosis and treatment services.
- If state law requires an in-person examination prior to the delivery of telemedicine services, the in-person services must be concluded and documented in the member’s medical record prior to the initiation of any related telehealth visits and issuance of prescriptions.
- For situations in which the standard of care requires an in-person examination in order to establish a diagnosis and determine recommended treatment, the in-person examination must be performed and documented in the member’s medical record prior to issuing a prescription via telemedicine.
- If allowable per state regulations, a provider without an established provider-patient relationship may issue a prescription via telemedicine if the prescribing provider is:
- Consulting at the request of another practitioner who maintains an ongoing relationship with the member;
- The other practitioner has performed an in-person physical examination of the member; and
- The other practitioner agrees to supervise the member’s ongoing care and use of the prescribed medications.
All federal and state prescribing statutes and regulations, including any limitations on prescribing and dispensing controlled substances, must be adhered to in prescribing through telemedicine technology.
American Well™ (Amwell) is the Highmark-approved vendor for Well360 Virtual Health, Highmark’s virtual care solution.
Effective Jan. 1, 2022, Highmark introduced a long-term virtual health platform, Well360 Virtual Health. To support our Well360 Virtual Health platform, we chose Amwell as our exclusive vendor solution, with Highmark and Amwell both sharing a goal of offering the ultimate member experience for virtual urgent and behavioral health care, virtual primary care, dermatology, and women’s health.
Well360 Virtual Health is easy to access and navigate when members need convenient, real-time virtual urgent care visits and virtual access to behavioral health.
Important: Teladoc will still continue to be available to some ASO (Administrative Services Only) clients.
Services Provided by Well360 Virtual Health
Well360 Virtual Health provides national coverage by certified providers via real-time interactive video and audio telecommunications technology. If members use Well360 Virtual Health for any of the following treatments, member cost sharing applies and can vary in the form of a copay or subject to network deductible and/or coinsurance as per their benefits:
- 24/7/365 Urgent Care: Urgent-type care, such as, but not limited to the following: cough, sinus infection, sore throat, vomiting, diarrhea, fever, pinkeye, flu/cold, headache. These practitioners belong to nationwide networks of licensed, board-certified physicians, including family practitioners, internists, and pediatricians for acute care for minor illness.
- See member's On-Demand Telemedicine Service benefit.
- Virtual Behavioral Health provided by Well360 Virtual Health. Scheduled video appointments, contingent upon provider availability, for conditions such as, but not limited to the following: Depression, anxiety, stress management, relationship challenges, child behavior difficulties and medication management. Therapy is for ages 10+ and Psychiatry services are available to ages 18+
- See member’s Outpatient Mental Health benefit.
- Virtual Primary Care: The Virtual Primary Care solution connects members to virtual primary care doctors, providing easy and fast access to care. Primary care visits are scheduled visits with the member’s virtual PCP. Pediatricians are available servicing children 12 and older. Primary Care appointments can typically be scheduled within seven days or less. Services include both medically necessary office visits and routine physical exams.
- See member’s PCP/Physician Office Visit benefit.
- Dermatology: The dermatology solution virtually connects a member to a dermatologist. This is done by secure asynchronous* capabilities which allow for more convenient skin examinations and faster turnaround times compared to in-person dermatology visits.
- See member’s Specialist Office Visit benefit.
- Women’s Health: Women’s Health provides services for women by providers who specialize in women’s care. Women’s Health service consists of three different services offered on the platform – Women’s Health Medical Care, Women’s Health Therapy (12 years+) and Women’s Health Lactation Consulting (16 years+).
- See member’s On-Demand Telemedicine Service, Outpatient Mental Health, and Preventive Adult Care benefit.
All vendors operate in accordance with state laws and regulations, and their providers are licensed to practice in the state in which the member is located. Members must have the benefit associated with the service line to obtain these services from Well360 Virtual Health.
IMPORTANT Well360 Virtual Health consists of providers within the Amwell Medical Group (AMG).
Each Well360 Virtual Health service line is housed within a member’s benefits. Urgent care within the On-Demand Telemedicine Service Benefit, Behavioral Health within Outpatient Mental Health, Primary Care under PCP/Physician Office Visit, Dermatology under Specialist Office visit, and Women’s Health (Medical Care under On-Demand Telemedicine Service, Therapy under Outpatient Mental Health, and Lactation under Preventive Adult Care).
For More Information
To learn more about Amwell, visit amwell.com.
Attention: Providers Using the Amwell Technology Platform for Their Private Practices
If you contract with American Well to provide an online virtual visit option for your patients using the Amwell technology platform, the agreement includes 24/7 support provided by Amwell’s nationwide provider network, the “Online Care Group,” whenever you/your staff are not available. Please keep in mind that Highmark member benefits may vary depending on who is actually performing the services:
- If you provide Virtual Outpatient Office Visits to Highmark members, the services are eligible under the Highmark member’s Office Visit benefits.
- If primary care services are provided to a Highmark member by an Amwell Online Care Group provider, they are eligible under a Highmark member’s On-Demand Telemedicine Service benefit, if applicable.
As a result, the Highmark member’s cost-sharing may vary depending on which provider performs the service — you or the Online Care Group. In addition, if the member does not have the On-Demand Telemedicine Service benefit, as well as other benefits (see above), the services would not be covered when provided by an Online Care Group provider.
In your discussions with Amwell, confirm that it will be clear to your patients who is providing care when they sign on for an online visit — you or the Online Care Group. In addition, educate your patients about your online access and availability, and ensure that your Highmark patients understand that their benefits/cost-sharing could differ if care is provided by the Online Care Group when you are not available.
Attention: Behavioral Health Providers
Virtual Behavioral Health visits, whether provided by you or by an Online Care Group provider, are subject to cost-sharing under the member’s Outpatient Mental Health benefit; therefore, the member’s cost-sharing is the same for services provided by you or by the Online Care Group.
For More Information on Other Telemedicine Services
Please see the applicable sections of this unit for more information on Highmark’s benefit enhancements that provide coverage for Virtual Outpatient Office Visits and Virtual Behavioral Health/Substance Abuse (Substance Use Disorder).
Virtual Visits provide our network participating providers with the option of delivering services to our members via real-time interactive audio and video telecommunications, or “telemedicine,” when appropriate. Telemedicine enables providers to extend their reach and improve their efficiency and effectiveness while still maintaining high quality care and attention to patient safety.
Virtual Visits are the remote delivery of outpatient services through the use of secure real-time interactive audio and video telecommunications technology. A patient can participate in a virtual visit with a provider from the privacy of their own home, office, or other private setting.
Why Virtual Outpatient Visits?
Virtual Visits can provide expanded access to services, more efficient delivery of services, and also potential cost savings.
- Access to care can be increased for all members — especially for individuals with multiple chronic health conditions, those with severe illness and disability, and underserved populations in rural and remote areas.
- Virtual visits are a cost-effective way to engage with patients and deliver care anywhere, anytime, while reducing administrative costs for the provider and travel costs for the patient.
- Virtual Visits can be used to triage cases and help reduce emergency room visits and hospitalizations by diverting members to less costly forms of care.
Originating and Distant Sites
The “originating site” is the location of an eligible member at the time the evaluation or consultation service is being provided via a virtual visit. The originating site can be either a medical site (e.g., PCP’s office, outpatient facility) or a non-medical site (e.g., member’s home or office) and is connected to a performing provider at a “distant site" (i.e., the performing provider’s physical location).
The virtual visit benefit provides coverage for the services of the performing provider at the distant site and also for an access fee billed by the medical originating site where the patient is located, when applicable.
Eligible Providers
Highmark participating providers who have the required telecommunications technology to support Virtual Visits are eligible. The services performed must fall under the scope of the provider’s license, and the sessions must be conducted following Highmark’s service and security guidelines.
Providing Virtual Visits for Highmark members is optional and not a requirement of network providers.
Member Eligibility
Virtual Visits are available to most Highmark members with individual health plans and employer group coverage, both fully and self-insured, that include benefits for Outpatient Office Visits. This is also available for Federal Employee Program (FEP) members.
Any member cost-sharing or visit limits under the Outpatient Office Visit benefit would apply. For example, if a member’s benefit has a copay for an office visit, then the copay would be applied to Virtual Visits.
Consult coverage materials to determine eligibility for Medicare Advantage and Medicare Supplemental plans.
Reminder: Always Verify Benefits
Providers are reminded to always verify a member’s eligibility and benefits prior to rendering services. It is the provider’s responsibility to confirm that the member’s benefit plan provides the appropriate benefits for the anticipated date of service. You can verify benefits electronically quickly and easily via Availity’s Eligibility and Benefits Inquiry or by submitting a HIPAA 270 transaction.
In Availity, use Additional Benefit Notes in Eligibility and Benefits Response.
If the member has coverage for Virtual Outpatient Office Visits, the benefit category will indicate "Virtual Visits – Yes."
Important: On-Demand Telemedicine Service Benefit Category is for Well360 Virtual Health and Teladoc Services Only
Virtual Visits are a service delivery option provided to our members under the Outpatient Office Visit benefits. They are separate from the services provided by our approved telemedicine vendors — Amwell and Teladoc, which are independent companies that provide online medical consultation services for patients through their network of practitioners.
In Availity's Eligibility and Benefits Inquiry, the “Telemedicine Service” benefit category under Professional Services is an indicator for Well360 Virtual Health and Teladoc services only. It does not indicate a member’s eligibility for Virtual Visits. For more information on the services these vendors provide for Highmark members, please see the section in this unit titled Services Provided by Well360 Virtual Health and Approved Vendors.
Note: Highmark partners with Amwell to deliver Well360 Virtual Health, Highmark’s virtual care solution.
Technology Requirements
The Virtual Visits must take place via real-time audio and video telecommunications. Interactive telecommunications technology must be multi-media communication that, at a minimum, includes audio and video equipment permitting real-time consultation among the patient location and provider location.
The provider must ensure that the aesthetic quality of the consultation is comparable to that of an in-person consultation (i.e., proper lighting, camera positioning, network connection, etc.). The provider’s monitor resolution (matrix) must be a minimum of 512x512 at 8-bit pixel depth.
The technology needed by the member will be driven by the technology platform that the provider uses to conduct this service. Members can be at any location that they choose that is conducive for Virtual Visits, provided the member has access to both audio and video streaming technology. The member should be in a location that is private and away from distractions.
Security Guidelines
Virtual Visits must be conducted through real-time interactive audio and video telecommunications hardware and software that are HIPAA (Health Insurance Portability and Accountability Act) and HITECH (Health Information Technology for Economic and Clinical Health Act) compliant.
Highmark supports the highest standards to protect the confidentiality of our members’ information, but there may be risks in passing personal health information (PHI) virtually. Highmark is not responsible for the security of virtual visits and does not validate the safeguards of any equipment and software used on either side of the virtual transmission.
Guidelines for Providing Services
Virtual Visits are not intended to replace in-person visits and support; it is another care delivery option that can be used by primary care providers if they choose. The provider can make the determination whether Virtual Visits are the right course of treatment for their patients. If you offer Virtual Visits but feel that it will not be the most effective approach for a patient, then you may refuse to see the patient virtually.
Virtual Visits can be conducted for initial, follow-up, or maintenance care; however, providers should give careful consideration in determining whether an in-person office visit for the initial visit would be beneficial in establishing a doctor-patient relationship.
Requirements
The following guidelines must be followed when conducting Virtual Visits:
- Telemedicine can be delivered via a real-time 2-way audio-only conversation in Delaware (DE), New York (NY), Pennsylvania (PA), and West Virginia (WV) – but in DE and NY, the patient must be unable to access the appropriate broadband service or other technology necessary to establish an audio and visual connection.
- All services provided must be medically necessary.
- Services performed must fall under the scope of the provider’s licensure.
- Providers shall comply with local, state, and federal laws and other regulatory agency requirements.
- Mechanisms to ensure continuity of care, follow-up, and referrals for emergency services must be in place and transparent to patients. Telemedicine treatment and consultations, including the authorization and dispensing of prescription medication(s), shall be held to the same professional standards of appropriate medical practice as those in a traditional in-office face-to-face encounter.
- The provider must take the appropriate steps to establish a doctor-patient relationship and conduct all appropriate evaluations and history consistent with traditional standards.
- The provider must obtain all relevant medical information (e.g., patient demographic information, chief complaint, history of present illness, allergies, medications, past medical/surgical/family history, and social history) prior to delivery of a medical diagnosis and treatment.
- Documentation of any visits using secure interactive audio and/or video telecommunications technology must be maintained in the patient’s medical record as required with in-person diagnosis and treatment services.
- When applicable, at a medical originating site, the medical examination of the patient at the originating site must be under the control of the specialty practitioner at the distant site.
- A designated room with appropriate equipment, including camera, lighting, transmission, and other needed electronics and the appropriate medical office amenities is established in both the medical originating site, when applicable, and the distant site.
Billing and Reimbursement
Claims for Virtual Visits are submitted based on how you are contracted with Highmark.
Reimbursement will be based on the plan allowance in place at the time services were rendered.
Member cost sharing (copay, deductible, and/or coinsurance) and visit limits apply if applicable.
For more information on billing and reimbursement, please see Highmark Reimbursement Policy 046: Telemedicine and Telehealth Services. Reimbursement policies are available on the Provider Resource Center by hovering over Claims in the main menu and choosing Reimbursement Policies under Reimbursement Resources.
Reminder: Directing Care to Network Providers
Providers are reminded that members will receive the highest level of benefits when a provider is a participating Highmark network provider and, when applicable, is in the highest benefit tier. Depending on their benefit plan, some members may not receive coverage for services provided by an out-of-network provider or may be responsible for higher cost-sharing amounts for services provided by an out-of-network provider.
As a participating provider, you should direct members to other providers who participate in the network associated with the member’s benefit plan. If a recommended provider is not participating in the network associated with the member’s benefit plan, the member must be notified in advance that a non-participating provider is not obligated to follow Highmark contractual guidelines and services could result in higher out-of-pocket expenses for the member.
The demand for behavioral health/substance abuse (substance use disorder) services continues to steadily increase. However, telemedicine is now allowing behavioral health/substance abuse (substance use disorder) specialists to provide their expertise remotely, offering more flexibility. Highmark will reimburse mental health/substance abuse (substance use disorder) providers for outpatient care delivery via Virtual Behavioral Health/Substance Abuse (Substance Use Disorder).
What is Virtual Behavioral Health/Substance Abuse (Substance Use Disorder)?
Virtual behavioral health/substance abuse (substance use disorder) is the remote delivery of outpatient mental health/substance abuse (substance use disorder) services through the use of secure real-time interactive audio and video telecommunications technology. A patient can participate in a virtual visit with a behavioral health/substance abuse (substance use disorder) specialist from the privacy of their own home, office, or other private setting.
Why Virtual Behavioral Health/Substance Abuse (Substance Use Disorder)?
Virtual behavioral health/substance abuse (substance use disorder) is about more than just convenience — it is about members receiving the care that they need when they need it, or the care they are afraid to seek in person due to social stigma. It helps address barriers to access, stigma, and time constraints typically associated with mental health/substance abuse (substance use disorder) services. Virtual behavioral health/substance abuse (substance use disorder) can provide expanded access to services, more efficient delivery of services, and also potential cost savings.
- Access to mental health/substance abuse (substance use disorder) care can be increased for all patients but especially for individuals with multiple chronic health conditions, those with severe illness and disability, and underserved populations in rural and remote areas.
- Virtual visits can provide added comfort to patients who otherwise might be fearful and resistant to meet face-to-face in a clinic.
- Counseling and intervention services can be delivered more quickly via teleconferencing sessions versus on-site appointments that may take longer to arrange.
- Virtual visits are a cost-effective way to engage with patients and deliver care anywhere, anytime while reducing administrative costs for the provider and travel costs for the patient.
- Virtual behavioral health visits can be used to conduct psychiatric consultations to triage cases and help reduce emergency room visits and hospitalizations by diverting clients to less costly forms of care.
Eligible Providers
Any Highmark participating mental health/substance abuse (substance use disorder) provider who has the necessary telecommunications technology to support a virtual outpatient mental health/substance abuse (substance use disorder) visit may participate. The services performed must fall under the scope of the provider’s license, and the sessions must be conducted following Highmark’s recommended service and security guidelines. Providing virtual behavioral health/substance abuse (substance use disorder) visits for Highmark members is optional and not a requirement.
Member Eligibility
Virtual behavioral health/substance abuse (substance use disorder) is available to most Highmark members with individual health plans and employer group coverage, both fully and self-insured, that include an Outpatient Mental Health/Substance Abuse (Substance Use Disorder) benefit. Note: If a member’s group plan does not include or carves out mental health/substance abuse (substance use disorder) benefits to a vendor, then Highmark’s virtual behavioral health/substance abuse (substance use disorder) coverage would not apply to the member.
Any member cost-sharing under the Outpatient Mental Health/Substance Abuse (Substance Use Disorder) benefit would apply. For example, if a member’s benefit plan has a copay for an outpatient mental health visit, the copayment will apply to virtual mental health services.
Virtual behavioral health services are not available for members with Medicare supplemental plans.
Note: This is also available for Federal Employee Program (FEP) members.
Important: On-Demand Telemedicine Service Benefit Category is for Well360 Virtual Health and Teladoc Services Only
Virtual behavioral health/substance abuse (substance use disorder) is a service delivery option provided to our members under the Outpatient Mental Health benefit. It is separate from the services provided by our approved vendors — Amwell and Teladoc — under the On-Demand Telemedicine Service benefit. Amwell and Teladoc are independent companies that provide online medical consultation services for patients through their network of practitioners.
In Availity's Eligibility and Benefits Inquiry, the "Telemedicine Service" benefit category under Professional Services is an indicator for Well360 Virtual Health and Teladoc services only. It does not indicate a member’s eligibility for virtual behavioral health services. For more information on the services these vendors provide for Highmark members, please see the section in this unit titled Services Provided by Well360 Virtual Health and Approved Telemedicine Vendors.
Note: Highmark partners with Amwell to deliver Well360 Virtual Health, Highmark’s virtual care solution.
Reminder: Always Verify Benefits
Providers are reminded to always verify a member’s eligibility and benefits prior to rendering services. It is the provider’s responsibility to confirm that the member’s benefit plan provides the appropriate benefits for the anticipated date of service. You can verify benefits electronically quickly and easily via Availity’s Eligibility and Benefits Inquiry or by submitting a HIPAA 270 transaction.
Technology Requirements
The virtual behavioral health/substance abuse (substance use disorder) visit must take place via real-time interactive video and audio telecommunications. Interactive telecommunications technology must be multi-media communication that, at a minimum, includes audio and video equipment permitting real-time consultation among the patient location and provider location.
The provider must ensure that the aesthetic quality of the consultation is comparable to that of an in-person consultation (i.e., proper lighting, camera positioning, network connection, etc.). The provider’s monitor resolution (matrix) must be a minimum of 512x512 at 8-bit pixel depth.
The technology needed by the member will be driven by the technology platform that the provider uses to conduct this service. Members can choose at any location that is conducive for virtual behavioral health/substance abuse (substance use disorder) visits, provided the member has access to both audio and video streaming technology. The member should be in a location that is private and away from distractions.
Security Guidelines
Virtual behavioral health/substance abuse (substance use disorder) visits must be conducted through real-time interactive audio and video telecommunications hardware and software that are HIPAA (Health Insurance Portability and Accountability Act) and HITECH (Health Information Technology for Economic and Clinical Health Act) compliant.
Highmark supports the highest standards to protect the confidentiality of our members’ information, but there may be risks in passing personal health information (PHI) virtually. Highmark is not responsible for the security of virtual visits and does not validate the safeguards of any of the equipment and software used on either side of the virtual transmittal.
Guidelines for Providing Services
Virtual visits are not intended to replace in-person visits and support; it is another care delivery option that can be used by mental health/substance abuse (substance use disorder) providers if they choose. The provider can make the determination whether a virtual behavioral health/substance abuse (substance use disorder) visit is the right course of treatment for their patients. The mental health/substance abuse (substance use disorder) provider must determine what channel of care is the best for their patient. If you offer virtual behavioral health/substance abuse (substance use disorder) services but feel that it will not be the most effective approach for a patient, then you may refuse to see the patient virtually.
Virtual behavioral health/substance abuse (substance use disorder) visits can be conducted for initial, follow-up, or maintenance care; however, providers should give careful consideration in determining whether an in-person office visit for the initial visit would be beneficial in establishing a doctor patient relationship.
The following guidelines must be followed when conducting virtual behavioral health/substance abuse (substance use disorder) visits:
Any telecommunications technology used must provide both audio and video streams that meet Highmark’s technology and security requirements.
- All services provided must be medically appropriate and necessary.
- Services performed must fall under the scope of the provider’s licensure.
- Providers shall comply with local, state, and federal laws and other regulatory agency requirements.
- Telemedicine treatment and consultations, including the authorization and dispensing of prescription medication(s), shall be held to the same professional standards of appropriate medical practice as those in a traditional in-office face-to-face encounter.
- The provider must take the appropriate steps to establish a doctor-patient relationship and conduct all appropriate evaluations and history consistent with traditional standards.
- The provider must have all the relevant medical information (e.g., patient demographic information, chief complaint, history of present illness, allergies, medications, past medical/surgical/family history, and social history) to deliver a competent medical diagnosis, treatment, and counseling plan.
- Documentation of the real-time interactive audio and video telecommunication relevant to the ongoing medical care of the patient should be maintained as part of the patient’s medical record.
- New York practitioners must provide Highmark current details on availability of their participating behavioral health/substance abuse (substance use disorder) services, including provider locations (city, town, and ZIP Code), for purposes of ensuring that Highmark at all times has the most current provider behavioral health/substance abuse (substance use disorder) service information.
Billing and Reimbursement
Reimbursement for virtual behavioral health/substance abuse (substance use disorder) service is based on the fee schedule in place on the date of service and is subject to any applicable member cost-sharing (copay, deductible, and/or coinsurance).
For more information on billing and reimbursement, please see Highmark Reimbursement Policy Bulletin RP-046: Telemedicine and Telehealth Services. Reimbursement policies are available on the Provider Resource Center by hovering over Claims in the main menu and choosing Reimbursement Policies under Reimbursement Resources.
The Highmark Provider Directory located on each of our public websites is a fast, easy way for our members to find providers near their homes or their workplace. And it is a valuable tool that offers your current and potential patients important details about your practice, including office location, hours of operation, parking availability, and nearby public transit information.
The online Provider Directory can also indicate if you are able to offer the “virtual” telemedicine services as described in this unit (Virtual Outpatient Office Visits; Virtual Behavioral Health/Substance Abuse (Substance Use Disorder) Visits; and for providers located in Delaware, telemedicine services as applicable under Delaware House Bill 69 and Delaware House Bill 160). This is self-reporting and up to you to supply us with this information.
Updating Your Practice Information via Availity Essentials®
If you are able to provide virtual visits/telemedicine services, you can notify Highmark by updating your practice information via Availity. Select Provider Data Maintenance or Provider File Management (Delaware, Pennsylvania, and West Virginia only) in Availity's Payer Spaces.
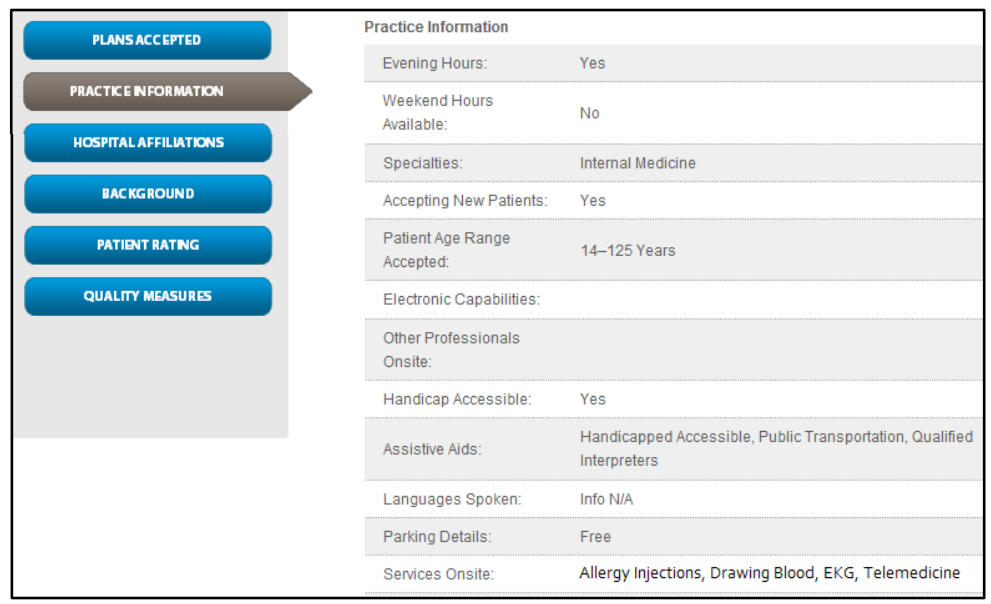
Once your files are updated, your listing in the online Provider Directory will be updated to indicate that you can provide telemedicine services. Here is an example of how this would display in Practice Information in your file of the Provider Directory:
What is Telestroke?
A telestroke service is a consultative modality that facilitates care for patients with acute stroke in a hospital emergency department by a vascular neurologist at stroke centers. These services are provided through telemedicine in the form of real-time video-conferencing for timely consultations with a vascular neurologist.
Telestroke services operate on a "hub and spoke" model allowing community hospitals that lack comparable staffing as larger urban hospitals and academic medical centers to access the expertise of the stroke centers and provide enhanced stroke care.
Applicable Products
The telestroke benefit enhancement applies to all eligible Highmark members with Commercial coverage.
Hub and Spoke
The "hub" is considered the specialist, the vascular neurologist at the stroke center. The specialist is able to visualize real-time video feeds and conduct examinations of patients experiencing stroke-like symptoms from various emergency departments that represent the "spoke" via a video-conference link.
Originating Site Billing and Reimbursement
When a "spoke" facility is providing a telestroke service via a telecommunications system, they are to use HCPCs code Q3014 (telehealth originating site facility code) to bill for the technical services, along with Revenue Code 0780 with a stroke diagnosis.
Always Check Medical Policy
Medical Policy includes medical guidelines that are appropriate for the majority of individuals with a particular disease, illness, or condition.
Highmark's medical policies are accessible on the Provider Resource Center in the main menu under Policies and Programs and then Medical Policies.
Verify Eligibility
Providers are reminded to always verify a member's eligibility and benefits prior to rendering services. It is the provider's responsibility to confirm that the member's benefit plan provides the appropriate benefits for the anticipated date of service.
You can verify benefits electronically quickly and easily via Availity's Eligibility and Benefits Inquiry or by submitting a HIPAA 270/271 transaction.
The following entities, which serve the noted regions, are independent licensees of the Blue Cross Blue Shield Association: Western and Northeastern PA: Highmark Inc. d/b/a Highmark Blue Cross Blue Shield, Highmark Choice Company, Highmark Health Insurance Company, Highmark Coverage Advantage Inc., Highmark Benefits Group Inc., First Priority Health, First Priority Life, Highmark Care Benefits Inc., or Highmark Senior Health Company. Central and Southeastern PA: Highmark Inc. d/b/a Highmark Blue Shield, Highmark Benefits Group Inc., Highmark Health Insurance Company, Highmark Choice Company or Highmark Senior Health Company. Delaware: Highmark BCBSD Inc. d/b/a Highmark Blue Cross Blue Shield. West Virginia: Highmark West Virginia Inc. d/b/a Highmark Blue Cross Blue Shield, Highmark Health Insurance Company or Highmark Senior Solutions Company. Western NY: Highmark Western and Northeastern New York Inc. d/b/a Highmark Blue Cross Blue Shield. Northeastern NY: Highmark Western and Northeastern New York Inc. d/b/a Highmark Blue Shield.
All references to “Highmark” in this document are references to the Highmark company that is providing the member’s health benefits or health benefit administration and/or to one or more of its affiliated Blue companies.
All revisions to this Highmark Provider Manual (the “manual” or “Highmark Provider Manual”) are controlled electronically. All paper copies and screen prints are considered uncontrolled and should not be relied upon for any purpose.