Unit 3: Medicare Advantage Procedures
5.3 Expedited Review of Initial Determinations and Appeals
5.3 Medicare Advantage Medical Policy
5.3 Advising Members of Their Inpatient Rights at Discharge
5.3 Notice of Medicare Non-Coverage (NOMNC)
5.3 Medicare Outpatient Observation Notice (MOON)
5.3 Preservice Organization Determinations
5.3 Non-Emergency Ambulance Transport
5.3 Authorization Requests for Outpatient Therapy Services
5.3 Medical Record Documentation Requirements
5.3 Chronic Care Management Services
This unit outlines Highmark and Centers for Medicare and Medicaid Services (CMS) procedures and processes specifically for Medicare Advantage members.
CMS Requirements Overview
CMS requires specific procedures for Medicare Advantage member notification and appeal processes to ensure that beneficiaries with coverage under a Medicare Advantage plan have adequate notice of appeal rights when coverage of their health care services is denied, reduced, or terminated.
When it has been determined that it is no longer medically necessary for a member to continue receiving care in a hospital, skilled nursing facility (SNF), from a home health agency (HHA), or from comprehensive outpatient rehabilitation facilities (CORFs), CMS requires the provider to notify that member of the termination of services and provide a statement of appeal rights.
In addition, CMS requires notification when it is deemed that services may be denied prior to the services being rendered and when Medicare beneficiaries, including Medicare Advantage, are receiving observation services as outpatients for more than 24 hours.
Compliance Terms
The regulations governing the Medicare Advantage program set forth required terms for both Medicare Advantage plans and contracted providers. To make contracted providers aware of such terms, CMS has created a contracting checklist for Medicare Advantage plans to follow in developing providers’ contracts and related policies and procedures.
In certain cases, regulatory language must be included in the actual contractual document governing the relationship between the Medicare Advantage plan and the provider. In other cases, CMS allows a Medicare Advantage plan to include required terms in its policies and procedures that are made available to contracted providers.
Highmark maintains a complete listing of the required Medicare Advantage compliance terms that may be included in Highmark’s policies and procedures. Highmark’s providers are required to comply with all such provisions.
Medicare Advantage compliance language can be found in the Appendix of the Highmark Provider Manual.
For More Information
To learn more about Highmark’s Medicare Advantage products, please see the Highmark Provider Manual Chapter 2 Unit 2: Medicare Advantage Products and Programs.
In addition, Member Evidence of Coverage (EOC) Booklets for Highmark Medicare Advantage plans are made available in the Appendix of the Highmark Provider Manual to assist you in servicing our Medicare Advantage members. The EOCs explains their rights, benefits, and responsibilities as a member of our Plan. The Appendix is available in the main Highmark Provider Manual in Chapter 7.
Providers should be knowledgeable about the expedited review of initial determinations and appeals for Highmark’s Medicare Advantage products. Although these processes are largely member-driven, the physician may represent the member and initiate the expedited review. Also, the physician is responsible for the crucial role of providing requested medical records on a timely basis.
When asking for an expedited review, the enrollee or the physician must submit either an oral or written request directly to the organization responsible for making the determination. The physician may also provide oral or written support for an enrollee’s own request for an expedited determination.
Background
The Centers for Medicare & Medicaid Services (CMS) requires all Medicare Advantage programs to implement processes for member-initiated expedited review of initial determinations and appeals. For its Medicare Advantage programs, Highmark has processes in place for expedited review of initial determinations and appeals for members with all Medicare Advantage products.
Highmark must automatically provide an expedited determination to any preservice or continued services request made or supported by a physician. The physician must indicate either orally or in writing that applying the standard time for making a determination could seriously jeopardize the life or health of the enrollee or the enrollee’s ability to regain maximum function. The physician need not be appointed as the enrollee’s authorized representative in order to make the request.
Expedited Review Rights
Members of Medicare Advantage programs, or their representatives, may request a 72-hour expedited review of a service if they believe the member’s health, life, or ability to regain maximum function may be jeopardized by waiting for the standard review process. In accordance with CMS guidelines, members may request the initial expedited review without speaking to the PCP first.
Highmark reserves the right to determine whether the request meets the criteria for an expedited review. Each appeal is processed in a manner consistent with the clinical urgency of the situation.
Not Applicable to Claim Denials
The processes for expedited review of initial determinations and appeals do not apply to claim denials if services have already been received. Members or providers may appeal claims denials through their respective standard appeal processes.
Your Role
You may be contacted by a Highmark staff member or physician advisor to supply a copy of the member’s medical records in the case of an expedited review. If so, you must supply the records immediately.
Additionally, if you are contacted for information by a Highmark physician advisor about an expedited appeal, you must return his/her call. Failure to do so could result in corrective action and/or sanctioning.
Appealing on Behalf of a Member
You or a treating physician may wish to initiate an appeal on behalf of a Medicare Advantage member if you believe services are medically necessary and covered under the member’s benefit plan.
If a Denial Decision is Upheld
If a denial decision is upheld on appeal, Highmark is required to forward the case to the CMS appeals contractor within 24 hours of the decision for Medicare Advantage (Part C).
The appeals contractor may request additional information. In such cases, a Highmark Medicare Advantage appeals staff member may contact your office for additional information. If you are contacted, please respond to the request immediately.
Note: For Part D prescription drug coverage, the member or provider must request an appeal through the CMS appeals contractor.
Expedited Review or Appeal Process
The table below explains the process for expedited reviews of initial determinations or appeals for Medicare Advantage members.
Note: Appeal administrators will automatically forward member appeals that do not meet expedited review criteria through the standard appeal process.
|
Step |
Who Does It… |
What Happens… |
|---|---|---|
|
1 |
Member or treating physician |
Decides to pursue an expedited initial determination or expedited appeal. |
|
2 |
Member |
Does member want to pursue the review or the appeal or appoint someone as a representative?
|
|
3a |
Member or Physician |
3a. For expedited appeals the member or the physician does not require a representative statement to make a request. Members or physicians may request an expedited review or appeal by phone, fax, or by mail. If an appeal request does not meet expedited criteria, it will be processed as a standard appeal. |
|
Or |
||
|
3b |
An appointed representative |
3b. The appointed representative may submit an Appointment of Representative (AOR) form by following instructions located on the form directly or sending a written equivalent. Both member and representative must sign the document. Fax or mail the signed document to the contact information in Step 4. |
|
4 |
Member or appointed representative |
Contacts the Expedited Review department at:
May send a physician’s statement supporting the urgent need for services to: Fax:
Mail:
|
|
5 |
Clinical Services care manager and/or physician reviewer |
Investigates the review (the 72-hour period begins upon receipt of this request). Is there enough information to render a decision?
|
|
6 |
Care provider |
Forwards member’s medical records to a Highmark staff member or physician advisor. |
|
7 |
Highmark care manager, medical appeals staff, and/or physician reviewer |
|
Where Can I Get Forms?
A current copy of the Appointment of Representative form (#CMS 1696) is always available under the CMS’ forms section of the CMS website here
The Centers for Medicare & Medicaid Services (CMS) requires that Medicare Advantage plans utilize National and Local Coverage Determinations (NCDs/LCDs) when providing indications and limitations of coverage.
NCD/LCD guidelines have been integrated into the claims processing system, allowing for cost-effective claims processing and ensuring consistent, accurate administration of our customers’ health care benefits.
Plan Exclusions and Restrictions
The following exclusions and restrictions apply to Highmark’s Medicare Advantage plans:
- Services considered not reasonable and necessary according to the standards of Original Medicare, i.e., Local and National Coverage Determinations (LCD/NDC), Healthcare Common Procedure Coding System (HCPCS), Current Procedural Terminology (CPT), and Current National Correct Coding Initiatives (NCCI), and/or other CMS guidance.
- Experimental medical and surgical procedures, equipment, and medication unless covered by Original Medicare, i.e., LCD/NDC, HCPCS, CPT, NCCI, and/or other CMS guidance.
Accessing Medicare Advantage Medical Policy
Prior to rendering service, it is important to review medical necessity criteria outlined in the Medicare Advantage Medical Policies that are available on CMS’ Medicare Coverage Database website. To access Highmark’s Medicare Advantage medical policies, go to the Provider Resource Center and click Policies & Programs > Medical Policies. Scroll down the page to Medicare Advantage Policy Search section.
Medicare Advantage plans must notify their members of their Medicare appeal rights at or near the time of a hospital or facility admission and discharge. The Centers for Medicare & Medicaid Services (CMS) policy requires acute care facilities to give all Medicare and Medicare Advantage inpatients the Important Message From Medicare (“Important Message”) no later than two days after admission to the inpatient level of care. A follow-up copy must also be delivered to the patient no more than two days prior to discharge.
The member will need to sign and date the Important Message to indicate that he/she received and understood it. The acute-care facility must then provide the member with the signed Important Message and retain a copy of the signed document in the member’s medical record.
Important Message
The Important Message explains the member's rights as an inpatient as well as his/her right to appeal a discharge decision. It also indicates the circumstances under which the member will or will not be liable for charges for continued stay in the acute-care facility. CMS requires facilities to maintain a copy of the signed Important Message in their files. This can be done electronically or via paper, according to each facility's standard record retention policy.
Process
The following steps are required for both medical and behavioral health services:
|
Step |
Action |
|---|---|
|
1 |
Give all Medicare Advantage inpatients the Important Message From Medicare at or near the time of admission, but no later than two days after admission to the inpatient level of care. |
|
2 |
Provide a follow-up signed copy of the Important Message From Medicare to all Medicare Advantage patients (or, if necessary, to their representative) prior to discharge, but no more than two days before discharge. Retain a copy of the signed document in the member’s medical record or in some other location/format to demonstrate that the requirement was met. |
Member Must Comprehend
The member must be able to understand the purpose and contents of the notice to be able to sign indicating receipt. The facility is responsible to explain the Important Message and to ensure that the member understands its content. Members who do understand must sign and date the form to indicate receipt and understanding.
If the facility determines that the patient does not understand that he/she can appeal the discharge decision, the facility must provide the Important Message document to another individual acting as the patient's representative. The representative must then sign and date it to indicate receipt and understanding.
If the member decides to accept the discharge, he/she leaves the facility and goes home or to an alternative level of care.
Member Disagrees with Discharge Decision
If the member disagrees with the discharge decision, he/she has until midnight on the day of the scheduled discharge (while he/she is still an inpatient) to decide to pursue an expedited review (appeal). If the member decides to pursue the appeal, additional steps are necessary.
This procedure applies only to patients who disagree with the discharge decision and wish to initiate an expedited review of the discharge decision:
|
Step |
Action |
|---|---|
|
1 |
If the patient disagrees with the discharge decision, no later than midnight on the day of discharge the patient or authorized representative contacts the Quality Improvement Organization (QIO) as directed on the Important Message From Medicare. |
|
2 |
The QIO notifies the facility and Highmark that the request was received. The QIO will notify the facility to forward relevant records and complete and deliver the Detailed Notice of Discharge. |
|
3 |
The facility will deliver the Detailed Notice of Discharge to the member no later than noon of the day the facility is notified of the review request. This notice provides the member with the clinical and coverage reasons why the member’s physician has determined that the level of care is no longer reasonable or medically necessary. The member is not required to sign this document. |
|
4 |
No later than one day after receiving all the necessary information, the QIO completes its review and communicates its decision to the member, facility, and the health plan. |
Timeline for Discharge Notification Process
For a detailed timeline for the delivery of the Important Message and Detailed Notice of Discharge, click here. The timeline outlines the responsibilities of each individual who has a role in the process.
If Member Disagrees with QIO Decision
If the Medicare Advantage member disagrees with an adverse QIO review decision, the member may request reconsideration while still an inpatient in the hospital.
Locating Forms
Current copies of the Important Message From Medicare and the Detailed Notice of Discharge are available on the CMS website.
In addition, a Highmark branded Detailed Notice of Discharge is available. This form can also be found on the Resource Center – select Resources & Education, then Miscellaneous Forms. Scroll to DETAILED NOTICE OF DISCHARGE.
For More Information
Beneficiary and Family Centered Care QIOs (BFCC-QIOs) handle case reviews. The BFCC-QIO for the region that includes Pennsylvania and West Virginia is Livanta.
Quality Innovation Network QIOs will offer health care quality improvement learning opportunities, technical assistance, and free resources to support providers. Quality Insights is the Quality Innovation Network-Quality Improvement Organization (QIN-QIO) that services Pennsylvania and West Virginia. For more information, please visit their website.
In addition, you may call Highmark’s Provider Service Center at:
- Delaware: Freedom Blue PPO: 800-346-6262
- New York: 800-329-2792
- Pennsylvania:
- Freedom Blue PPO: 866-588-6967
- Community Blue Medicare HMO: 888-234-5374
- Community Blue Medicare PPO and Plus PPO: 866-588-6967
- Security Blue HMO (Western Region only): 866-517-8585
- West Virginia: Freedom Blue PPO: 888-459-4020
- New York: 800-329-2792
Procedure for SNFs, HHAs, and CORFs
The CMS also requires skilled nursing facilities (SNFs), home health agencies (HHAs), and comprehensive outpatient rehabilitation facilities (CORFs) to follow special procedures to ensure that Medicare Advantage patients are given adequate notice of discharge and appeal rights.
The Centers for Medicare & Medicaid Services (CMS) requires skilled nursing facilities (SNFs), home health agencies (HHAs), and comprehensive outpatient rehabilitation facilities (CORFs) to follow special procedures to ensure that Medicare Advantage patients are given adequate notice of discharge and appeal rights. The member must be given appropriate notice when it has been determined that coverage of their health care services is denied, reduced, or terminated.
CMS has issued a Notice of Medicare Non-Coverage (NOMNC) form that providers must use to notify both Medicare beneficiaries and enrollees of Medicare Advantage plans that Medicare coverage for specific services currently being received will end.
The CMS is requiring that insurers, including Highmark, collect additional documentation from facilities for Quality Improvement Organization (QIO) program audits, effective Jan. 1, 2024.
For these audits, facilities will now be required to submit the following forms to the health plan when they are issued:
- Notice of Medicare Non-Coverage (NOMNC)
- Detailed Explanation of Non-Coverage (DENC)
The NOMNC form is available on the Provider Resource Center . See the “Locating the Form” section below. The DENC form is available on the CMS website by clicking here. Completed forms should be faxed to Highmark at this number: 888-740-4318.
Time Frame
The NOMNC form should be issued no later than two days before the proposed end of services.
Valid Delivery
Valid delivery means that the member or appointed or authorized representative* must be able to understand the purpose and contents of the notice to sign for receipt of it. The member, or appointed or authorized representative, must be able to understand that he/she may appeal the termination decision. If the member, or appointed or authorized representative, is not able to comprehend the contents of the notice, it must be delivered to and signed by a representative.
*An appointed or authorized representative requires an AOR (Appointment of Representative Form) or a POA (Power of Attorney).
Valid Delivery Methods
The NOMNC form can be delivered using the following methods:
- In person to a member, or appointed or authorized representative; or
- Via telephone when unable to provide the NOMNC form to the member, or appointed or authorized representative, in person.
If the NOMNC form is delivered by telephone, then the facility must confirm the telephone contact by acknowledging the conversation in writing and mailing it on the same day.
Important
Providers cannot leave any of this information in a voicemail message. CMS considers only direct verbal notifications to be valid.
Provider Information Required
The provider must document the name, address, and telephone number of the provider delivering the notice at the very top of the first page of the form. The field for this information is located immediately below the logo of the product under which the member has coverage. The form is not considered valid without this information.
Providers choosing to use a NOMNC form that is not specifically branded for Highmark products must add their name, address, and telephone number in this same location on the first page of the form.
Additional Information Section
Highmark has chosen to add fields in the "Additional Information" section for the provider to document the details supporting the valid delivery of the notice. This documentation is designed to protect the provider, the member, and the health plan, especially when the notice must be delivered to a member's representative who is not physically present in the facility. The facts required in the Additional Information section of the form are as follows:
- Details of the conversation with the member or representative;
- The name and telephone number of the Quality Improvement Organization (QIO);
- The date and time by which the QIO must be contacted;
- The name and title of the individual delivering the NOMNC to the member or representative on behalf of the facility;
- The date and time of the conversation during which the NOMNC was delivered to the member or representative;
- The method of delivery (verbal, telephonic, etc.);
- If delivered by telephone, also include the telephone number called; and
- The date on which written confirmation was sent as follow up to telephone delivery.
Note: Although some of these fields are most immediately applicable to situations in which the NOMNC is delivered to a member or representative not present in the facility, the relevant information should be documented in all cases.
Telephone Delivery: Obtaining the Member's Signature
When the NOMNC form is delivered via telephone, the member's signature can be obtained as follows:
- The member or representative may come to the facility to sign the NOMNC form at a later date; or
- The facility should make a copy of the NOMNC form for the facility's records, and then send the original to the member or representative via certified mail requesting that a receipt be returned to the facility if the member or representative is unable to come to the facility for signature.
Retain Copy
Facilities should retain a copy of the completed and signed NOMNC form in their records.
Locating Form
The Notice of Medicare Non-Coverage form applicable to Highmark Medicare Advantage plans is located on the Provider Resource Center's Miscellaneous Forms page. Scroll to the Notice of Medicare Non-Coverage heading to access the form.
Congress passed the Notice of Observation Treatment and Implication for Care Eligibility (NOTICE) Act, which requires all hospitals and critical access hospitals (CAHs) to provide written and oral notification to all Medicare beneficiaries receiving observation services as outpatients for more than 24 hours. The written notice must include the reason the individual is receiving observation services and must explain the implications of receiving outpatient observation services, in particular the implications for cost-sharing requirements and subsequent coverage eligibility for services furnished by a skilled nursing facility.
Medicare Outpatient Observation Notice (MOON)
The Medicare Outpatient Observation Notice (MOON) was developed by the Centers for Medicare & Medicaid Services (CMS) to serve as the standardized written notice. The MOON must be presented to Medicare beneficiaries, including those with Medicare Advantage plans, to inform them that the observation services they are receiving are outpatient services and that they are not an inpatient of the hospital or CAH. Hospitals and CAHs must deliver the notice no later than 36 hours after observation services are initiated or sooner if the individual is transferred, discharged, or admitted. The hospital or CAH must obtain the signature of the patient or a person acting on behalf of the patient (“representative”) to acknowledge receipt of the notification. If the individual or representative refuses to sign it, the written notification is signed by the hospital staff member who presented it.
To Access the MOON Form
The CMS approved standardized MOON form (CMS-10611) and accompanying instructions are available on the CMS website.
The Medicare Advantage member has a right to an advance determination by their health plan to verify whether services are covered prior to receiving the services. In circumstances where there is a question whether or not an item or service is covered under a member’s Medicare Advantage benefit plan, a provider must advise the member to request a preservice organization determination from their health plan, or the provider can request the determination on the member’s behalf.
If coverage for the item or service is denied, the health plan must provide the member with a standard written denial notice that states the specific reasons for the denial and informs the member of his/her appeal rights.
Note: The Advance Beneficiary Notice of Noncoverage (ABN) used for the Original Medicare program is not applicable to Medicare Advantage plans.
Notification of Non-Coverage Determinations
Giving a preservice denial notice to members in advance of performing a service is not compliant with CMS regulations for Medicare Advantage plans.
The notification of a non-coverage determination must be issued to the member by Highmark. If you believe that a service or item is not covered or may not be covered for a Highmark Medicare Advantage member, you must advise the member that a written coverage decision (“preservice organization determination”) is required from Highmark before the service or item can be provided.
Exceptions to Preservice Organization Determination Requirements
Preservice organization determinations are not required for Highmark Medicare Advantage members receiving the services listed below. These services are clearly listed as exclusions for Medicare Advantage members in Highmark’s Evidence of Coverage (EOC) booklets.
- Private duty nurses.
- Personal items in member’s room at a hospital or a skilled nursing facility, such as a telephone or television.
- Full-time nursing care in the member’s home.
- Custodial care provided in a nursing home, hospice, or other facility setting when the member does not require skilled medical care or skilled nursing care. Custodial care is personal care that does not require the continuing attention of trained medical or paramedical personnel, such as care that helps the member with activities of daily living, such as bathing or dressing.
- Homemaker services including basic household assistance, including light housekeeping or light meal preparation.
- Fees charged by member’s immediate relatives or members of the member’s household.
- Meals delivered to the member’s home.
- Radial keratotomy, LASIK surgery, vision therapy, and other low vision aids.
- Reversal of sterilization procedure and non-prescription contraception supplies.
- Naturopath services (uses natural or alternative therapies).
- Services provided to veterans in Veterans Affairs (VA) facilities.
- Chiropractic care, other than manual manipulation of the spine consistent with Medicare coverage guidelines.
- Orthopedic shoes, unless the shoes are part of a leg brace and are included in the cost of the brace or the shoes are for a person with diabetic foot disease.
- Medical determination of refractive state (Medical Refraction).
The services listed above are not eligible for payment and can be billed to the member.
Important: Providers are required to direct members to obtain or request a preservice organization determination prior to the receipt of all non-covered services other than those listed above. Failure to obtain a Notice of Denial of Medical Coverage will result in the member being held harmless from any payment liability.
Requesting Preservice Organization Determinations
Highmark members can be directed to call the Member Service phone number on the back of their identification card to initiate a preservice organization determination. Or, if you prefer to act on behalf of the member, you should call Highmark Provider Services as follows:
- Delaware: Freedom Blue PPO: 800-346-6262
- New York: 800-329-2792
- Pennsylvania:
- Freedom Blue PPO: 866-588-6967
- Community Blue Medicare HMO: 888-234-5374
- Community Blue Medicare PPO and Plus PPO: 866-588- 6967
- Security Blue HMO (Western Region only): 866-517-8585
- West Virginia: Freedom Blue PPO: 888-459-4020
Note: This process is not applicable to services or items that require prior authorization. Requests for prior authorization are to be submitted via Availity®.
Time Frame for Reviews (PA Only)
Upon receipt of a request for a coverage determination, Highmark will review the request and provide notification of the decision as quickly as the member’s health condition requires.
For a standard non-urgent request, Highmark will notify the member of the determination within 14 calendar days after receiving the request. Highmark will extend the time frame up to 14 calendar days if the member requests an extension, or if Highmark can justify a need for additional information and can document how the delay is in the best interest of the member. For example, the receipt of additional medical evidence from a noncontracting provider may change Highmark’s decision to deny.
In cases involving the need for urgent care, Highmark will provide notification of the decision within 72 hours after receipt of the request. A case involving urgent care is one in which making the determination under the standard time frames could seriously jeopardize the member’s life, health, or ability to regain maximum function or, in the opinion of a physician with knowledge of the member’s medical condition, would subject the member to severe pain that could not be adequately managed without the care or treatment that is the subject of the request. If a physician indicates a case as one involving urgent care, it will be handled as such.
For non-participating providers, Highmark will extend the urgent case turnaround time of 72 hours or the non-urgent case turnaround time of 14 calendar days up to an additional 14 calendar days if the member requests the extension. Contracted providers are obligated under the terms of their contract to respond to requests from the Plan for the purpose of reviewing a member’s appeal.
For non-participating providers, Highmark may also extend the urgent 72 hour or non-urgent 14 calendar time frames up to an additional 14 calendar days if a need for additional information can be justified and it is documented that the delay is in the interest of the member. Contracted providers are obligated under the terms of their contract to respond to requests from the Plan for the purpose of reviewing a member’s appeal.
Time Frame for Reviews
Upon receipt of a request for a coverage determination, Highmark will review the request and provide notification of the decision as quickly as the member’s health condition requires.
For a standard non-urgent request, Highmark will notify the member of the determination within seven calendar days after receiving the request. Highmark will extend the time frame up to seven business days if the member requests an extension, or if Highmark can justify a need for additional information and can document how the delay is in the best interest of the member. For example, the receipt of additional medical evidence from a noncontracting provider may change Highmark’s decision to deny.
In cases involving the need for urgent care, Highmark will provide notification of the decision within two calendar days after receipt of the request. A case involving urgent care is one in which making the determination under the standard time frames could seriously jeopardize the member’s life, health, or ability to regain maximum function or, in the opinion of a physician with knowledge of the member’s medical condition, would subject the member to severe pain that could not be adequately managed without the care or treatment that is the subject of the request. If a physician indicates a case as one involving urgent care, it will be handled as such.
For non-participating providers, Highmark will extend the urgent case turnaround time of two calendar days or the non-urgent case turnaround time of sevencalendar days. Contracted providers are obligated under the terms of their contract to respond to requests from the Plan for the purpose of reviewing a member’s appeal.
For non-participating providers, Highmark may also extend the urgent two calendar day or non-urgent seven calendar day timeframes. Contracted providers are obligated under the terms of their contract to respond to requests from the Plan for the purpose of reviewing a member’s appeal.
Notice of Denial of Medical Coverage
If a review results in a non-coverage determination, Highmark will issue a Notice of Denial of Medical Coverage. This standardized written notice will state the specific reasons for the denial and inform the member of his/her appeal rights.
When a provider initiates a coverage determination on behalf of a member, the provider will receive a copy of the Notice of Denial of Medical Coverage that is issued to the member.
If the member initiated the coverage determination, the Notice of Denial of Medical Coverage will be issued to the member. The provider will receive a copy of the notice issued to the member, provided that Highmark is able to obtain the provider’s information at the time the request is made.
Prior authorization from Highmark is required for non-emergent ambulance transports for Highmark Medicare Advantage plan members in Delaware, Pennsylvania, and West Virginia.
All non-emergent ambulance transportation, whether a one-time trip or scheduled repetitive transports, require prior authorization from Highmark, with the exception of non-emergent transports originating at a hospital (inpatient discharge, ER discharge).
When non-emergent ambulance trips originate at a hospital (i.e., inpatient discharge, ER discharge), the hospital/facility may serve as a delegate and authorize the transport without having to obtain prior authorization from Highmark.
Note: This exception does not apply to hospital-based treatments, such as dialysis and cancer treatment; transports to and from ongoing hospital-based treatment (e.g., dialysis, chemotherapy) require prior authorization from Highmark.
Medical Necessity Criteria
Non-emergent ambulance transportation is covered under Highmark’s Medicare Advantage plans if it meets the Centers for Medicare & Medicaid Services (CMS) medical necessity guidelines. Non-emergent transportation by ambulance is appropriate if the member (beneficiary) is bed-confined. This means the member meets all three of the following CMS criteria for bed confinement:
- is unable to get up from bed without assistance;
- is unable to ambulate; and
- is unable to sit in a chair or wheelchair
Or
The member’s condition is such that other means of transportation (Access, wheelchair/stretcher vans, taxi, personal vehicle) could endanger the member’s health and, therefore, ambulance transport is medically necessary.
Available Procedure Codes
The following HCPCS codes for non-emergent ambulance transports are subject to prior authorization as per the requirements above:
- A0426 – Ambulance service, Advanced Life Support (ALS), nonemergency transport, Level 1
- A0428 – Ambulance service Basic Life Support (BLS), non-emergency transport
Requesting Authorization
The treating provider is responsible for obtaining prior authorization, and the ambulance provider is responsible for verifying that the service was authorized. Requests for prior authorization should be submitted via Availity Essentials.
Decision Notification
Highmark will make a determination within 48 hours of receiving the request. The ordering/treating provider will be notified of the decision by the method used to submit the request. Decision letters are sent via mail to the ambulance provider and to the member.
Authorizations will provide confirmation of the ambulance provider, transport origin and destination, number of transports approved, and start/end dates. If authorization is denied, the decision letter will provide a detailed written explanation outlining which specific policy requirements were not met.
Prior Authorization Not Required
- Prior authorization is not required for:
- Emergent transportation
- Transports originating from a hospital setting (i.e., inpatient discharge, ER discharge). This does not include hospital-based treatments (i.e., dialysis, cancer treatment) that do require prior authorization from Highmark.
Speech Therapy
For Medicare Advantage members, speech therapy requires authorization to begin treatment. The authorization requests for speech therapy are reviewed by Highmark’s Clinical Services department. Your authorization requests for speech therapy services can be submitted to Highmark via Availity.
Note: Clinical Services reserves the right to request a full plan of treatment as deemed necessary.
Telephone Requests
If you are not yet Availity-enabled, authorization requests for speech therapy for Medicare Advantage members can be submitted to Highmark by contacting Clinical Services at:
Delaware Freedom Blue PPO: 800-346-6262
New York: 800-329-2792
Pennsylvania:
- Freedom Blue PPO: 866-588-6967
- Community Blue Medicare HMO: 888-234-5374
- Community Blue Medicare PPO and Plus PPO: 866-588-6967
- Security Blue HMO (Western Region only): 866-517-8585
West Virginia Freedom Blue PPO: 800-269-6389
The authorization request to begin treatment must be initiated by the member’s physician who is requesting the therapy services.
Highmark participating providers are expected to maintain a single standard medical record in such form and containing such information as required by all applicable federal and state laws that govern operations and all applicable Highmark policies and procedures.
Documentation Requirements
For each encounter, Medicare Advantage medical records must include, but not be limited to, all the following:
- Documentation that is appropriate and legible to someone other than the writer.
- Appropriate, timely, and legible provider signatures and credentials on the documentation.
- Date of service (or review for consultation, laboratory, or testing report) clearly documented in the medical record which correlates to the date of reported claim.
- Documentation supporting the need for the service reported on the claim.
- The member’s name (on each page) and date of birth.
CMS Signature and Credentials Requirements
CMS has stated that stamped signatures are not acceptable on any medical records. The prohibition applies to all providers who bill the Medicare Program. CMS will accept handwritten signatures, electronic signatures, or facsimiles of original written or electronic signatures.
CMS also requires that the provider of service for face-to-face encounters must be appropriately identified on medical records via their signature and physician credentials.
Compliance
If a provider fails to comply with these documentation requirements, remedial actions such as rejection of claims, review of claims on a retrospective basis and collection of any overpayments, and/or termination of provider agreements as noted in the provider contract may be initiated as appropriate.
Acceptable Provider Signatures
Valid provider signatures include:
- electronic signatures which include credentials;
- handwritten signatures including credentials;
- printed name including credentials accompanied by provider initials; and
- facsimiles of original written or electronic signatures that include credentials.
Type and Acceptable:
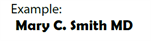
Hand-written signature including credentials
- Mary C. Smith, MD; or MCS, MD
Examples:

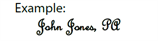
Electronic signature, including credentials
- Requires authentication by the responsible provider
Examples include but are not limited to:
“Approved by,” “Signed by,”
“Electronically signed by”
- Must be password protected and used exclusively by the individual provider
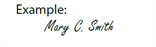
Printed name including credentials, accompanied by handwritten initials

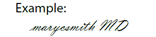
Facsimile
- Other than an original signature, such as included on medical record copy
Invalid Provider Signatures
The following table provides information on invalid provider signatures:
Type
- Typed name with credentials
Unacceptable Unless..
- The provider includes a written signature or initials plus credentials
Type
- Non-physician or non-physician extender signature (e.g., medical student)
Unacceptable Unless..
- Co-signed by supervising physician
(Refer to acceptable examples in the preceding table.)
Type
- Provider of services signature without credentials
Unacceptable Unless..
- Name is linked to provider credentials or name with credentials on practitioner stationery
Type
- Signature stamp, including credentials
Unacceptable Unless..
- Prior to 2008
(Stamped signatures are not permitted on medical records after 2008.)
Highmark complies with, and requires its contracted providers to comply with, CMS policies and procedures including inspection of records.
Record retention is required to ensure efficient availability in case of immediate need. Compliance with CMS’ requirements is paramount for continuing participation in the Medicare Advantage program and the ability to service our Medicare Advantage members.
Policy
CMS revised its regulations with respect to records retention and access to records, increasing the period from six to ten years. Therefore, network providers must maintain records and information in an accurate and timely manner in accordance with 42CFR §422.504(d) and provide access to such records in accordance with 42CFR §422.504(e)(2).
42CFR §422.504(d) states Medicare Advantage organizations are to maintain records and allow CMS access to them for ten years from the termination date of the contract or the date of the completion of any audit.
42CFR §422.504(e)(2) states:
“HHS, the Comptroller General, or their designees may audit, evaluate, or inspect any books, contracts, medical records, patient care documentation, and other records of the Medicare Advantage organization, related entity, contractor, subcontractor, or its transferee that pertain to any aspect of services performed, reconciliation of benefit liabilities, and determination of amounts payable under the contract, or as the Secretary may deem necessary to enforce the contract.”
If you wish to read the entire context of the requirement please visit The Code of Federal Regulations, Title 42, Volume 2, Chapter 1V – Centers for Medicare & Medicaid Services, Department of Health and Human Services, Part 422, Medicare Advantage Program, Subpart K, Contracts with Medicare Advantage Organizations.
CMS recognizes Chronic Care Management (CCM) as a critical component of primary care that contributes to better health and care for individuals.
Under the Medicare Physician Fee Schedule (PFS), Medicare pays separately for CCM services furnished to Medicare patients with multiple chronic conditions.
Definition
CCM services encompass the oversight and education activities by health care professionals to help patients with chronic diseases and health conditions, such as but not limited to, fibromyalgia, diabetes, sleep apnea, multiple sclerosis, lupus, and high blood pressure, to better understand their condition and successful management of it.
Highmark Reimbursement Policy Bulletin RP-043
Highmark follows CMS published guidelines for chronic care management services for Medicare Advantage as per Highmark Reimbursement Policy RP-043: Care Management.
These guidelines are available in the CMS Medicare Learning Network (MLN) booklet on Chronic Care Management Services.
Network providers are required to comply with the requirements of this section with respect to their Highmark Medicare Advantage patients. Providers are urged to adhere to these same standards with respect to their other Highmark patients in all types of plans.
Definitions
An advance directive is written instructions, such as a living will and medical (or durable) power of attorney, recognized under state law and signed by a patient, that explains the patient’s wishes concerning the provisions of health care if the patient becomes incapacitated or is unable to make those decisions known.
An advance directive can tell physicians and family members what life-sustaining treatments one does or does not want at some future time if one becomes incapable of making or communicating treatment decisions. An essential component of the advance directive is the selection of a person to make health and personal care decisions for one who lacks sufficient capacity to make or communicate choices.
A living will is a witnessed, notarized statement by which an individual specifies in advance what life-prolonging measures or other medical care he/she wants, or does not want, in the event the individual:
- is certified by one or more examining physicians to have a terminal condition or to be in a persistent vegetative state; and
- is unable to communicate his/her wishes.
A medical (or durable) power of attorney is a witnessed, notarized statement by which an individual appoints someone (typically a family member or trusted friend) to make health care decisions on the individual’s behalf in the event that the individual becomes unable to make such decisions. If called to act, the appointed representative is to make decisions consistent with the wishes and values of the incapacitated individual, and to act in the individual’s best interest where such wishes are unknown.
Some advance directives combine the functions of both a medical power of attorney and a living will.
Policy
Primary care physicians/practitioners (PCPs) must ask Medicare Advantage program members whether they have executed an advance directive and selected a surrogate. PCPs must then review the advance directive and determine their role as described in the procedure below.
Advance directive discussions must be documented in a prominent place in the medical record. A copy of the executed advance directive must be placed in a prominent part of the medical record.
If a provider cannot implement an advance directive, in whole or in part, as a matter of conscience, then the provider must:
- Issue a clear and precise written statement of this limitation, describing the range of medical conditions or procedures affected by the conscientious objection; and
- Discuss this with the patient and document the discussion in a prominent part of the individual’s medical record; and assist the member in locating another network provider, if the member so desires, or contact Highmark Customer Service at the telephone number located on the back of the member’s ID card so that we may assist in locating another network provider.
A provider may not condition the provision of care or otherwise discriminate against a Medicare Advantage member based on whether or not the individual has executed an advance directive.
Monitoring
During an office site visit, a nurse from Quality Management will review medical records to determine whether:
- Discussion of the advance directive with the member is documented in a prominent part of the medical record; and
- A copy of the advance directive, signed by the member and physician, is on file, if applicable.
Clinical studies may also be conducted to evaluate ongoing use and discussion of advance directives.
Procedure
|
Step |
Action |
|---|---|
|
1 |
Ask the member whether he/she has executed an advance directive. Document the response in the member’s chart.
|
|
2 |
Review the advance directive.
|
|
3 |
If possible, notify the member of the decision not to honor the advance directive. Member Service will make every effort possible to place the member with another provider who is able to honor the member’s wishes. |
Highmark West Virginia Responsibilities
Highmark Senior Solutions Company, through Highmark West Virginia, provides Freedom Blue Medicare Advantage members, at the time of initial enrollment, written information on their rights to make decisions concerning their medical care, including the right to accept or refuse medical or surgical treatment and the right to formulate advance directives.
Members are informed that complaints alleging denial of care or provision of care not authorized by an advance directive, or discrimination based on the existence of a directive, may be filed with the West Virginia Bureau of Public Health, Office of Health Facility Licensure and Certification at 304-558-0050.
Highmark West Virginia may monitor compliance with this section by review of a provider’s medical records during a site visit.
WV Forms and Additional Information
Select the appropriate link for copies of forms recognized under West Virginia law:
- State of West Virginia Medical Power of Attorney
- State of West Virginia Living Will
- State of West Virginia Combined Medical Power of Attorney & Living Will
For additional copies or more information about advance directives in West Virginia, providers may contact the following:
- West Virginia Bureau of Senior Services at 304-558-3317; or
- West Virginia Center for End-of-Life Care at 877-209-8086.
Providers may direct their patients who request additional information about advanced directives to the West Virginia Bureau of Senior Services or the West Virginia Center for End-of-Life Care at the numbers listed above or to similar other state agencies for members residing outside of West Virginia.
Additional Information About Advance Directives
Providers should contact their state health department, professional licensing board, health facility licensing agency, Medicare survey and certification agency, or legal counsel to learn the requirements for advance directives in their state and to obtain forms, if available.
Providers can direct their Highmark members to contact Blues on Call at 888-258-2428 for general (not state-specific) educational information on advance directives.
End stage renal disease (ESRD) is permanent kidney failure that requires kidney dialysis or a transplant to maintain life. Medicare beneficiaries generally cannot join a Medicare Advantage plan if they have this condition. However, if they develop this condition while they are a Medicare Advantage member, they will continue to be enrolled. It is important to identify all members with ESRD as soon as possible to ensure adequate treatment. Your role in identifying members with ESRD is crucial.
Policy
When a Medicare Advantage patient is determined to have chronic kidney failure and receives treatment in a Medicare-approved dialysis center or receives a kidney transplant, the attending physician should help the dialysis center complete an ESRD Medical Evidence Report, CMS-2728-U3.
It takes approximately four months for the CMS-2728-U3 forms to be processed through all systems to set up the initial record and pay appropriate reimbursement rates for members with ESRD. However, it is the responsibility of the patient’s dialysis center to send completed CMS-2728-U3 forms to the ESRD Network Organizations in a timely manner.
Procedure
|
Step |
Action |
|---|---|
|
1 |
The physician ordering dialysis contacts the dialysis center. |
|
2 |
The dialysis center is responsible for submitting the original copy of the completed CMS-2728-US to the servicing Social Security office. The dialysis center also submits copies of and is responsible for verifying the information on the form and resolving any questionable items before sending the information to the ESRD networks that transmit the information to CMS. |
|
3 |
The information that CMS receives from the ESRD Network Organizations is documented in CMS’s Group Health Plan system (GHP) which is responsible for assigning ESRD status. |
The following entities, which serve the noted regions, are independent licensees of the Blue Cross Blue Shield Association: Western and Northeastern PA: Highmark Inc. d/b/a Highmark Blue Cross Blue Shield, Highmark Choice Company, Highmark Health Insurance Company, Highmark Coverage Advantage Inc., Highmark Benefits Group Inc., First Priority Health, First Priority Life, Highmark Care Benefits Inc., or Highmark Senior Health Company. Central and Southeastern PA: Highmark Inc. d/b/a Highmark Blue Shield, Highmark Benefits Group Inc., Highmark Health Insurance Company, Highmark Choice Company or Highmark Senior Health Company. Delaware: Highmark BCBSD Inc. d/b/a Highmark Blue Cross Blue Shield. West Virginia: Highmark West Virginia Inc. d/b/a Highmark Blue Cross Blue Shield, Highmark Health Insurance Company or Highmark Senior Solutions Company. Western NY: Highmark Western and Northeastern New York Inc. d/b/a Highmark Blue Cross Blue Shield. Northeastern NY: Highmark Western and Northeastern New York Inc. d/b/a Highmark Blue Shield.
All references to “Highmark” in this document are references to the Highmark company that is providing the member’s health benefits or health benefit administration and/or to one or more of its affiliated Blue companies.
All revisions to this Highmark Provider Manual (the “manual” or “Highmark Provider Manual”) are controlled electronically. All paper copies and screen prints are considered uncontrolled and should not be relied upon for any purpose.