Unit 5: 1500 Claim Form Guidelines
The 1500 Health Insurance Claim Form (“1500 Claim Form”) answers the needs of many health care payers. It is the basic claim form required by many payers for paper claims submitted by physicians and other professional providers. And now that electronic claim submission has become integral to health care, many of the software/hardware systems used by providers for submitting electronic claims depend on the existing 1500 Claim Form in its current image.
Prior to the development of the 1500 Claim Form, there was no standardized form for physicians and other health care providers to report health care services. In the 1980’s, the American Medical Association (AMA), the Centers for Medicare & Medicaid Services (CMS; formerly known as HCFA), and many other payer organizations worked together through a group called the Uniform Claim Form Task Force to standardize and promote the use of a universal health claim form. As a result of this joint effort, the 1500 Claim Form is accepted nationwide by most insurance entities as the standard claim form/attending physician statement for submission of medical claims.
The Uniform Claim Form Task Force was replaced by the National Uniform Claim Committee (NUCC) in the mid-1990s. The NUCC continues to be responsible for the maintenance of the 1500 Claim Form. The official 1500 Health Insurance Claim Form data specifications are available through NUCC at nucc.org.
1500 Claim Form - 02/12 Version
Highmark accepts only the 02/12 version of the 1500 Claim Form. Photocopies, discontinued, or outdated versions of the 1500 Claim Form, including the 08/05 version, will not be accepted and will be returned to providers. Please remember that only original red claim forms will be accepted.
Photocopies of the 1500 Claim Form will not be accepted and will be returned to providers.
This tip sheet is designed to highlight the fields of the CMS-1500 (02/12) claim form that are required when submitting to Highmark.
Electronic Claims Submission
Highmark encourages providers who are submitting paper claims to consider electronic claims submission. Electronic transactions and online communications have become integral to health care. Today’s technology can help you simplify business operations, cut costs, and increase efficiency in your office.
Electronic claims submission is a valuable method of streamlining claim submission and processing, and results in faster payment. Highmark supports a variety of HIPAA-compliant electronic claims and inquiry transactions. Please refer to Chapter 1.3: Electronic Solutions – EDI & Availity for information on how to take advantage of the electronic solutions available to you.
You may also want to consider Availity® for submitting claims to Highmark. Availity is provided to Highmark network participating providers at no cost. This Internet-based service seamlessly integrates all insurer-provider transactions into one system — HIPAA-compliant claims submission, claim status inquiry, claim investigation, eligibility, benefits, and much more! Availity even provides access to Highmark’s tools for real-time claim estimation and adjudication. Additional information about Availity is also available in Chapter 1.3: Electronic Solutions – EDI & Availity.
OCR Scanner Improves Paper Claims Processing Time
Highmark uses an OCR (Optical Character Recognition) scanner for direct entry of paper claims into its claims processing system, OSCAR (Optimum System for Claims Adjudication and Reporting). OCR technology is an automated alternative to manually entering claims data. The OCR equipment scans the claim form, recognizes and “reads” the printed data, and then translates it into a format for direct entry into OSCAR. The scanner can “read” both computer-prepared and typewritten claim forms but only if the data is within the borders of each box.
Direct entry of claims by the OCR scanner is an advantage to you because it requires less human intervention in preparing and entering your claims. The scanner reads, numbers, and images your paper claims in one step. OCR scanning reduces claim entry time as well as entry errors. However, OCR claims do not receive the same priority processing as do electronically submitted claims.
For the most efficient processing, please use only original red 1500 Health Insurance Claim Forms. The OCR scanner is programmed to read this form. Highmark will not accept photocopies or discontinued versions of the 1500 Claim Form and will return claims received on these invalid forms. Providers will need to resubmit returned claims on valid, original forms for the claims to be entered into Highmark’s claims processing system.
If you use computer billing software to complete the 1500 paper claim forms, please remember to use original, current versions of the form and not photocopies or older versions of the claim form.
How to Obtain Claim Forms
To obtain a supply of the current version of the 1500 Health Insurance Claim Form, please contact:
- Your current forms supplier; or
- TFP Data Systems: e-mail 1500form@tfpdata.com, or telephone 800-482-9367, ext. 58029; or
- The Government Printing Office: http://bookstore.gpo.gov/catalog/government-forms-phone-directories, or telephone 866-512-1800.
In today’s business world, there are no requirements to submit claims on paper. In fact, Highmark’s claim system places higher priority on processing and payment of claims filed electronically. However, if you are submitting paper claims, the guidelines provided below must be followed when completing the 1500 Health Insurance Claim Form. By following these guidelines, you can be assured that your claims will be scanned as quickly as possible, processed accurately, and paid without delay.
Note: Please be sure to reference Chapter 6.1: General Claim Submission Guidelines for general guidelines and reporting tips that apply to claims submissions in both paper and electronic formats.
Be Sure to Use the Correct Forms
Highmark will accept only the Version 02/12 1500 Health Insurance Claim Form. Always provide Highmark with the original red 1500 form. Do not send copies or forms printed in black ink on a laser printer – they cannot be scanned. Photocopies, discontinued, or outdated versions of the 1500 Claim Form will not be accepted and will be returned to providers. Resubmission on a valid form will be required.
Appropriate Printing of Forms
Always print or type all information on the claim form. Clear, concise reporting on the form helps us to interpret the information correctly.
- Use computer-printed forms or type the data within the boundaries of the boxes provided. Do not handwrite.
- Use black ink. Do not use red ink. The OCR image scanner cannot read red ink.
- Printing Specifications:
- Use 10-pitch PICA type.
- Submit all claims on 20-pound paper.
- Do not use highlighters to emphasize information on the claim form or attachments. Highlighted information becomes blackened out when imaged and is not legible.
If Multiple Forms are Necessary
In cases where you must use several claim forms to report multiple services for the same patient, total the charges on each form separately. Treat each form as a separate and complete request for payment. Do not carry balances forward. It also is important that you report all other essential information on each claim form.
Complete the claim form in its entirety. Our claims examiners review each claim individually. If you submit several claim forms for the same member but fill in only essential details on one form, Highmark will reject the claim forms.
We must have complete information before we can process the claim. If details are missing, Highmark will reject the claim.
Use the Appropriate Mailing Address
Mail the claim forms to the appropriate P.O. Box address. A complete listing of addresses can be found in Chapter 1.2: Online Resources & Contact Information.
ICD-10 Compliance
For dates of service Oct. 1, 2015, and after, Highmark will accept ICD-10-CM diagnosis codes only on claims.
Diagnosis Code Reporting Guidelines for the 1500 Claim Form (02/12)
The following diagnosis code reporting guidelines are for all lines of business:
- Report diagnosis codes to the highest level of specificity available.
- The “ICD Indicator” identifies the version of the ICD code set being reported. Enter the applicable ICD indicator: 0 (zero) for ICD-10-CM. Enter the indicator between the vertical, dotted lines in the upper right-hand portion of the field.
- Enter the codes to identify the patient’s diagnosis and/or condition.
- Claims must be submitted with ICD-10-CM diagnosis codes.
- The lines allow for diagnosis codes at a maximum of seven characters.
- You may report a maximum of 12 diagnosis codes.
- Report only one diagnosis code on each line (labeled A-L) in Box 21 of the 02/12 1500 Claim Form.
- Enter the diagnosis codes left-justified on each line.
- Do not include the decimal point within the diagnosis code.
- Do not provide narrative description in this field.
- Relate lines A - L to the lines of service in 24E by the letter of the line.
- Substantiate all member diagnoses in the medical record.
For Medicare Advantage members:
In addition to above, include all diagnosis codes that impact the patient’s evaluation, care, and treatment for the current problems.
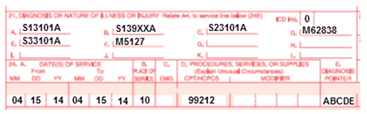
1500 Claim Form (02/12) Reporting Example
This is an example of reporting ICD-10-CM diagnosis codes on the 02/12 version of the 1500 Claim Form.
The additional tips provided here will help to ensure your claims submissions are completed accurately and to avoid any delays in processing. If you have a question about how to complete a claim form, contact Highmark’s Provider Service.
Before You Begin…
Always verify the patient’s information via Availity® or the HIPAA 270/271 Health Care Eligibility Benefit Inquiry and Response transaction before completing the claim form. Availity’s Eligibility and Benefits Inquiry function and the HIPAA 270/271 allow you to quickly confirm the member’s coverage and the member information needed on the claim form.
General Tips for Completing the Claim Form
- Please do not staple over the Quick Response (QR) code symbol at the top of the Version 02/12 1500 Claim Form. Highmark’s scanners read the symbol to identify that the 1500 Claim Form is the 02/12 version.
- Be certain to enter information within the correct fields on the form.
- Make sure that the member’s identification number is correctly reported on the claim form (including the alphabetical prefix).
- Use an 8-digit format for reporting date of birth (MMDDYYYY).
- Submit a separate claim for each patient even when they are members of the same family. When a patient has had multiple hospital admissions, submit separate claim forms for each hospital admission.
- Include coordination of benefits or Medicare information on the claim form when the patient qualifies.
- Always report your 10-digit NPI in Item Number 33a.
- Regularly change your printer’s ink cartridge or typewriter ribbon to ensure print readability. Light print cannot be read by the scanner.
- Avoid using special characters such as dollar signs, hyphens, slashes, or periods.
- Avoid extra labeling in fields on claim form.
- Use X’s for marking Yes or No blocks. Do not use other alphabetical indicators such as Y for Yes, N for No, F for Female, or M for Male.
- Do not use correction fluid on the claims.
- Leave the upper right-hand corner of the claim form blank for internal purposes. If you need to print information at the top of the form, use the open space in the center.
- If using a rubber stamp, do not stamp information in or over fields one through 33 or in the upper right corner of the claim form. Any stamps used should be in black ink only.
- Claims and other documents (inquiries, referrals, etc.) should never be taped or glued in any way. Staples should be avoided unless absolutely necessary.
When Completing Service Lines…
- Include the date each service was provided in 6-digit format (MM|DD|YY).
- Be certain the total charge equals the service line charges.
- Do not fill in blank fields or space with unnecessary data. For example, if hospitalization dates are not required, leave the field blank rather than entering 00/00/00 or XX/XX/XX.
- Include HCPCS codes to identify the service or services rendered. Other coding manuals may use the same code number to describe a different service.
- The claim form can only accommodate six lines of service. The top area of the six service lines is shaded and is the location for reporting supplemental information. Supplemental information can only be entered with a corresponding, completed service line. It is not intended to allow the billing of 12 lines of service.
- Report all information about a service on one line. If the service dates, diagnosis code, charge, etc., are reported on separate lines, the scanner “creates” an extra line. This may cause the claim to be returned to you for correction and re-submission.
- Use the procedure code that most closely describes the service. Written descriptions are only necessary if using NOC codes or when no procedure code is available. Unnecessary descriptions are problematic for OCR scanned claims.
- Not Otherwise Classified (NOC) Codes: When reporting NOC procedure codes, provide a written description of the item or service above the code in the shaded area of the service line on the claim form. When more than one NOC is submitted, provide an individual description and charge for each item. If an NOC code is reported when a more appropriate code is available, the claim will be rejected and requested to be resubmitted with correct information. The member should not be billed.
Tips for Specific Reporting Needs
- Surgical procedures do not require operative notes unless:
- An “individual consideration” (IC) or “unlisted procedure” code is reported.
- The service performed is a new procedure.
- The service performed is potentially cosmetic.
- Multiple primary surgeons participated in a surgical procedure.
- The terminology for the reported code indicates, “by report” (BR).
- A pre-authorization letter advised you to submit specific reports.
- The service involves unusual circumstances. Remember to also report modifier 22. If this modifier is not reported, the special circumstances will not be considered.
- When reporting circumcision for a baby boy, report the service on the baby’s claim, not the mother’s.
- When reporting services involving a multiple birth, report the services under the babies’ names, not as Baby A, Baby B, etc.
Avoid Including Unnecessary Attachments
- Do not submit a photocopy of the member’s identification card.
- Do not routinely send “Release of Information” forms signed by the patient. Our member agreements give us the right to receive the information without additional release forms.
- Avoid the use of Post-it Notes on claims or inquiries. (Full sheets of paper are preferable.)
- Avoid routinely attaching hospital notes (progress notes and order sheets) to claims. We will request this information if it is necessary to process the claim.
- Avoid routinely submitting copies of your payment records or ledgers. They often omit vital information and it may be difficult to determine what services are to be considered for payment.
- The OCR scanner is designed to read computer-prepared or typewritten claim forms. Claims with superbill attachments cannot process through the OCR scanner. Type data from the superbill directly onto the claim form. Do not attach superbills for the same services you have reported on the claim form.
Mailing Tips
- Use flat envelopes for mailing claims.
- Do not fold claim forms. Folded or wrinkled claim forms cannot be effectively read by the scanner.
Examples of How to Submit Information Correctly
|
Insured’s ID Number |
|---|
|
Correct: YYZ123456789001 |
|
Incorrect: YYZ-123-456-789001; ID # YYZ123456789001 |
|
Charges |
|---|
|
Correct: 20.00 |
|
Incorrect: $20.00 |
|
Date of Birth: 8-Digit Format |
All Other Dates: 6-Digit Format |
|---|---|
|
Correct: 12271949 |
Correct: 122713; 021414 |
|
Incorrect: 12/27/49; 12-27-1949 |
Incorrect: 12/27/13; 2-14-14 |
|
Insured’s Policy Group Number |
|---|
|
Correct: 123456; NAS123 |
|
Incorrect: GRP # 123456; GRP # NAS123 |
For More Information
For instructions on how to begin to submit claims electronically, visit the EDI Trading Partner website by clicking the applicable link below:
Or, you may call EDI Operations at 800-992-0246.
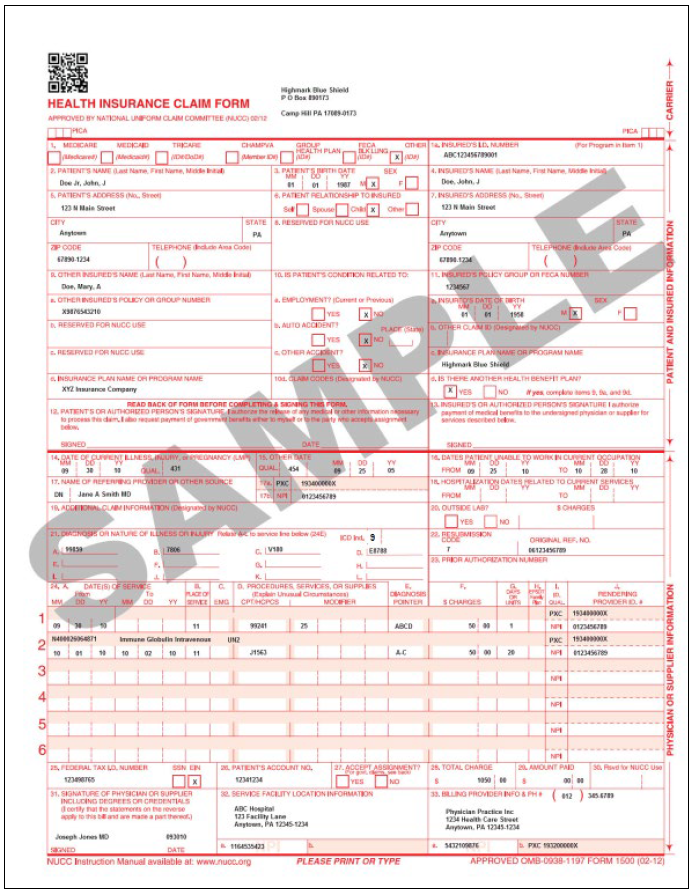
The National Uniform Claim Committee (NUCC) released the 02/12 version of the 1500 Health Insurance Claim Form (“02/12 1500 Claim Form”) in January 2014.
The instructions for completing the 1500 (02/12) paper claim form begin below. A “completed” 02/12 1500 Claim Form example is available at the end of this unit.
Important! Version 02/12 Required
Highmark will accept only the 02/12 version of the 1500 Claim Form. Also, please remember that only original red claim forms will be accepted (except in New York where both red and photocopies are acceptable). Photocopies, discontinued, or outdated versions of the 1500 Claim Form will not be accepted and will be returned.
Instructions for Completing the 1500 Claim Form Version (02/12)
Any data (e.g., diagnosis codes, charges, NPIs, etc.) used in the instructions and sample claim form is demonstrating how to enter data in the field and is not providing instruction on how to bill for certain services.
Note: Please refer to Chapter 6.4: Professional (1500/837P) Reporting Tips for additional information about specific claim reporting situations.
This tip sheet is designed to highlight the fields of the CMS-1500(02/12) claim form that are required when submitting to Highmark.
|
Item # |
Field Title /Description |
Instructions |
|
|---|---|---|---|
|
Top of Form |
Carrier Block |
Report name and address in the center of the open space. Do not report above Item #1a (this is where Highmark prints the claim number). Please do not staple over the Quick Response (QR) code symbol. Highmark’s scanners read the symbol to identify that the 1500 Claim Form is the 02/12 version. |
|
|
1 |
Type of Health Insurance |
For Highmark products, place an X in the "Other" box. |
|
|
1a |
Insured’s ID Number |
Enter insured's identification number exactly as shown on the insured's identification card. Be sure to include any alpha prefixes. |
|
|
2 |
Patient’s Name |
Enter the patient's full last name, first name, and middle initial. Use commas to separate the last name, first name, and middle initial. A hyphen can be used for hyphenated names. Do not use periods within the name. If the patient uses a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. Titles (e.g., Sister, Capt, Dr) and professional suffixes (e.g., PhD, MD, Esq) should not be included with the name. |
|
|
3 |
Patient’s Birth Date, |
Enter the patient's 8-digit birth date (MM|DD|YYYY). Enter an X in the correct box to indicate sex of the patient. Only one box can be marked. If gender is unknown, leave blank. |
|
|
4 |
Insured’s Name |
Enter the insured's full last name, first name, and middle initial. Use commas to separate the last name, first name, and middle initial. A hyphen can be used for hyphenated names. Do not use periods within the name. Do not use terms such as “Self” or “Same” if the patient is also the Insured. If the insured uses a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. Titles (e.g., Sister, Capt, Dr) and professional suffixes (e.g., PhD, MD, Esq) should not be included with the name. |
|
|
5 |
Patient’s Address |
Enter the patient's mailing address. This field has 3 lines — the first line is for the street address; the second line, the city and state; and the third line, the ZIP Code. “Patient’s Telephone” is not used in processing and is not required by Highmark. Do not use punctuation (i.e., commas, periods) or other symbols in the address (e.g., 123 N Main Street 101 instead of 123 N. Main Street, #101). Report a 5 or 9-digit ZIP Code. Enter the 9-digit ZIP Code without the hyphen. |
|
|
6 |
Patient Relationship to Insured |
Enter an X in the correct box to indicate the patient's relationship to insured. Only one box can be marked. |
|
|
7 |
Insured’s Address |
Enter the insured's address. If Item #4 is completed, then this field should also be completed. This field has 3 lines — the first line is for the street address; the second line, the city and state; and the third line, the ZIP Code. “Insured’s Telephone” is not used in processing and is not required by Highmark. Do not use punctuation (i.e., commas, periods) or other symbols in the address (e.g., 123 N Main Street 101 instead of 123 N. Main Street, #101). Report a 5 or 9-digit ZIP Code. Enter the 9-digit ZIP Code without the hyphen. |
|
|
8 |
Reserved for NUCC |
Highmark does not need this information to adjudicate the claim. Leave blank. |
|
|
9 |
Other Insured’s Name |
If Item #11d is marked, complete fields 9 and 9a-d; otherwise leave blank. When additional group health coverage exists, enter other insured’s full last name, first name, and middle initial of the enrollee in another health plan if it is different from that shown in Item #2. Use commas to separate the last name, first name, and middle initial. A hyphen can be used for hyphenated names. Do not use periods within the name. If the insured uses a last name suffix (e.g., Jr, Sr), enter it after the last name and before the first name. Titles (e.g., Sister, Capt, Dr) and professional suffixes (e.g., PhD, MD, Esq) should not be included with the name. |
|
|
9a |
Other Insured’s Policy or Group Number |
Enter the policy or group number of the other insured. |
|
|
9b |
Reserved for NUCC |
Highmark does not need this information to adjudicate the claim. Leave blank. |
|
|
9c |
Reserved for NUCC |
Highmark does not need this information to adjudicate the claim. Leave blank. |
|
|
9d |
Insurance Plan Name or Program Name |
Enter the other insured's insurance plan or program name. |
|
|
10a,b,c |
Is Patient’s Condition Related to: |
When appropriate, enter an X in the correct box to indicate whether one or more of the services described in Item #24 are for a condition or injury that occurred on the job or as a result of an automobile or other accident. Only one box on each line can be marked. The 2-letter state code (e.g., PA, DE) must be shown if "YES" is marked in Item #10b for "Auto Accident." Any item marked "YES" indicates there may be other applicable insurance coverage that would be primary, such as automobile liability insurance. |
|
|
10d |
Claim Codes (Designated by |
Highmark requires the sub-set of Condition Codes approved by the NUCC in this field, when applicable. When reporting more than one code, enter three blank spaces and then the next code. The Condition Codes approved for use on the 1500 Claim Form are available at http://www.nucc.org under Code Sets. |
|
|
11 |
Insured’s Policy, Group, or FECA Number |
Enter the insured's policy or group number as it appears on the insured's health care identification card. Do not use a hyphen or space as a separator within the policy or group number. If Item #4 is completed, then this box should also be completed. |
|
|
11a |
Insured’s Date of Birth, Sex |
Enter the 8-digit date of birth (MM|DD|YYYY) of the insured and an X to indicate the sex of the insured. Only one box can be marked. If gender is unknown, leave blank. |
|
|
11b |
Other Claim ID |
Highmark does not need this information to adjudicate the claim. Leave blank. |
|
|
11c |
Insurance Plan Name or Program Name |
Enter the insurance plan or program name of the insured. |
|
|
11d |
Is There Another Health Benefit Plan? |
When appropriate, enter an X in the correct box. If marked “YES”, complete 9, 9a, and 9d. Only one box can be marked. |
|
|
12 |
Patient’s or Authorized Person’s Signature |
Highmark does not need this information to adjudicate the claim. The “Patient’s or Authorized Person’s Signature” indicates there is an authorization on file for the release of any medical or other information necessary to process and/or adjudicate the claim. You may report "Signature on File," "SOF," or a legal signature in this box. If you obtain a legal signature, (1) be sure the name is contained inside this box so it does not interfere with data you report in other boxes, and (2) enter the date signed in 6-digit format (MM|DD|YY). If there is no signature on file, leave blank or enter "No Signature on File." |
|
|
13 |
Insured’s or Authorized Person’s Signature |
Highmark does not need this information to adjudicate the claim. The “Insured’s or Authorized Person’s Signature” indicates that there is a signature on file authorizing payment of medical benefits. You may report "Signature on File," "SOF," or a legal signature in this box. If you obtain a legal signature, (1) be sure the name is contained inside this box so it does not interfere with data you report in other boxes, and (2) enter the date signed in 6-digit format (MM|DD|YY). If there is no signature on file, leave blank or enter "No Signature on File." |
|
|
14 |
Date of Current Illness, Injury, or Pregnancy (LMP) |
Enter the 6-digit (MM|DD|YY) date of the first date of the present illness, injury, or pregnancy. For pregnancy, use the date of the last menstrual period (LMP) as the first date. Be sure to complete this field when services were performed as a result of accident or injury. Enter the applicable qualifier to identify which date is being reported:
Be sure to enter the date and qualifier in the correct fields. The qualifier is entered to the right of the vertical, dotted line. |
|
|
DE Only: For physical, occupational, and speech therapy services: This box must be completed if the Highmark Delaware member has a per condition benefit. |
|||
|
15 |
Other Date |
Enter another date related to the patient’s condition or treatment. Enter the date in the 6-digit format (MM|DD|YY). (Previous pregnancies are not a similar illness.) Leave blank if unknown.
Be sure to enter the date and qualifier in the correct fields. The qualifier is entered between the left-hand set of vertical, dotted lines. |
|
|
DE Only: For physical, occupational, and speech therapy services: Please provide date if applicable. |
|||
|
16 |
Dates Patient Unable to Work in Current Occupation |
If the patient is employed and is unable to work in current occupation, a 6-digit (MM|DD|YY) date must be shown for the "from-to" dates that the patient is unable to work. An entry in this field may indicate employment-related insurance coverage. |
|
|
17 |
Name of Referring |
Enter the name (first name, middle initial, last name) and credentials of the professional who referred or ordered the service(s) or supply(s) on the claim. Do not use periods or commas. A hyphen can be used for hyphenated names. If multiple providers are involved, enter one provider only using the following priority order:
Enter the applicable qualifier to identify which provider is being reported.
Enter the qualifier to the left of the vertical, dotted line. |
|
|
17a |
Other ID# |
When the Referring Provider’s National Provider Identifier (NPI) is associated with more than one Highmark-assigned provider number, the Provider Taxonomy Code correlating to the contracted specialty must be submitted in addition to the NPI. This enables the accurate application of the provider’s contractual business arrangements with Highmark. The PXC Provider Taxonomy qualifier is reported in the qualifier field to the immediate right of the box containing “17a,” followed by the referring Provider’s taxonomy code. |
|
|
17b |
NPI# |
Enter the NPI number of the referring provider, ordering provider, or other source in Item #17b. |
|
|
18 |
Hospitalization Dates |
Enter the inpatient 6-digit (MM|DD|YY) hospital admission date followed by the discharge date (if discharge has occurred). If not discharged, leave discharge date blank. This date is when a medical service is furnished as a result of, or subsequent to, a related hospitalization (inpatient services only). |
|
|
19 |
Additional Claim |
Highmark does not need this information to adjudicate the claim. Leave blank. |
|
|
20 |
Outside Lab?$Charges |
Highmark does not need this information to adjudicate the claim. Leave blank. |
|
|
21 |
Diagnosis or Nature of Illness or Injury |
The “ICD Indicator” identifies the version of the ICD code set being reported. Enter 0 (zero) for ICD-10-CM. Enter the indicator between the vertical, dotted lines in the upper right-hand area of the field. *************** In A – L, enter the codes to identify the patient’s diagnosis and/or condition. List no more than 12 diagnosis codes. Use the highest level of specificity. Enter the codes left-justified on each line. Do not include the decimal point within the diagnosis code. Relate lines A – L to the lines of service in 24E by the letter of the line. ** Do not provide narrative description in this field. ** Please see instructions regarding Federal Employee Program (FEP) claims and anesthesia reporting in Chapter 6.4: Professional (1500/837P) Reporting Tips. |
|
|
22 |
Resubmission |
When resubmitting a claim, enter the appropriate bill frequency code left justified in the left-hand side of the field.
List the original reference number for resubmitted claims. |
|
|
23 |
Prior Authorization |
For ambulance services, use this block to report the ZIP Code of the Point of Origin. (The 9-digit ZIP+4 Code is not required for the Point of Origin but will be accepted if reported.) Ambulance providers who submit paper claims for non-emergent ambulance transports must attach a PMNC (Physician’s Medical Necessity Certification) form to the claim. |
|
|
24 |
Supplemental information can only be entered with a corresponding, completed service line. The six service lines in section 24 have been divided horizontally to accommodate submission of both the NPI and another/proprietary identifier and to accommodate the submission of supplemental information to support the billed service. The top area of the six service lines is shaded and is the location for reporting supplemental information. It is not intended to allow the billing of 12 lines of service. The following types of supplemental information and their qualifiers can be entered in the shaded lines of Boxes 24A through 24H: |
||
|
Qualifier |
Type of Information |
||
|
7 Anesthesia information |
Report the surgical HCPC procedure code when a ‘Not Otherwise Specified’ or ‘Not Otherwise Classified’ anesthesia service is reported. A complete description of the surgical service performed can be used in lieu of a surgical HCPC code or if the only applicable surgical procedure code is an NOC. |
||
|
ZZ Narrative description of unspecified code |
Narrative description of unspecified code. |
||
|
N4 National Drug Codes (NDC) |
National Drug Codes (NDC) for drugs: Report the qualifier, N4, prior to the 11-digit* NDC, e.g., N499999999999. |
||
|
To enter supplemental information in the shaded area, begin at Box 24A by entering the qualifier and then the information. Do not enter a space between the qualifier and the number/code/information. Do not enter hyphens or spaces within the number/code. *Many NDCs are displayed on drug packaging in a 10-digit format. Proper billing of an NDC requires an 11-digit number in a 5-4-2 format. Converting NDCs from a 10-digit to 11-digit format requires a strategically placed zero, dependent on the 10-digit format. For more information, refer to the section titled Reporting National Drug Codes in Chapter 6.2: General Claim Submission Guidelines. |
|||
|
24A |
Date(s) of Service |
Enter date(s) of service, from and to, in 6-digit format (MM|DD|YY). If one date of service only, enter that date under "From." Leave "To" blank. If grouping services, you may range date if the place of service, procedure code, charges, and individual provider for each line is identical for that service line. Grouping is allowed only for services on consecutive days. The number of days must correspond to the number of units in Item #24G. An exception to this is prolonged detention care. Do not range date these services even when performed on consecutive days. |
|
|
24B |
Place of Service |
Enter the appropriate 2-digit code from the Place of Service Code list for each item used or service performed. The Place of Service Codes are available at: |
|
|
24C |
EMG |
Highmark does not need this information to adjudicate the claim. Leave blank. |
|
|
24D |
Procedures, Services, or Supplies |
Enter the CPT or HCPCS code(s) and modifier(s) (if applicable) from the appropriate code set in effect on the date of service. This field accommodates the entry of one procedure code and up to four 2-character modifiers. The specific procedure code(s) must be shown without a narrative description. |
|
|
24E |
Diagnosis Pointer |
In 24E, enter the diagnosis code reference letter (pointer) as shown in Item Number 21 to relate the date of service and the procedures performed to the primary diagnosis. When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow. The reference letter(s) should be A – L or multiple letters as applicable. Enter letters left justified in the field. Do not use commas between the letters; hyphens can be used for ranges of multiple letters. This field allows for the entry of 4 characters in the unshaded area. Diagnosis codes must be entered in Item Number 21 only. Do not enter them in 24E. |
|
|
24F |
$ Charges |
Enter the charge for each listed service. Enter the number right-justified in the left-hand area of the field. Do not use commas or dollar signs when reporting the dollar amount. Do not report negative dollar amounts. Enter 00 in the right-hand area of the field if the amount is a whole number. |
|
|
24G |
Days or Units |
Enter the number of days, units, or minutes. This field is most commonly used for multiple visits, units of supplies, anesthesia minutes, or oxygen volume. If only one service is performed, the numeral 1 must be entered. When required by payers to provide the NDC units in addition to the HCPCS units, enter the applicable NDC units' qualifier and related units in the shaded line following the NDC qualifier and code. The following qualifiers are to be used when reporting an NDC quantity. Report the qualifier prior to the quantity, e.g., UN2. |
|
|
F2 International Unit |
ML Milliliter |
||
|
GR Gram |
UN Unit |
||
|
24H |
EPSDT/Family Plan |
Highmark does not need this information to adjudicate the claim. Leave blank. |
|
|
24I |
ID Qualifier |
The ‘NPI’ ID qualifier is pre-populated in the non-shaded area of Item #24I. (The Rendering Provider’s NPI is reported in the non-shaded area of Item #24J.) When the Rendering Provider’s National Provider Identifier (NPI) is associated with more than one Highmark-assigned provider number, the Provider Taxonomy Code correlating to the contracted specialty must be submitted in addition to the NPI. This enables the accurate application of the provider’s contractual business arrangements with Highmark. When required to report the Rendering Provider’s Taxonomy Code, enter the PXC Provider Taxonomy qualifier in the shaded area of Item #24I. Note: In most instances, the 3-character PXC qualifier can be printed within Item #24I. If the PXC qualifier runs into Item #24J, our Optical Character Recognition (OCR) scanner will still capture the qualifier and provider taxonomy correctly since 24I and 24J are read as one field. |
|
|
24J |
Rendering Provider ID# |
The Rendering Provider is the person or company (laboratory or other facility) who rendered or supervised the care. Report the provider’s information in Item Numbers 24I and 24J only when different from data recorded in Item Numbers 33a and 33b. In other words, when you report a billing provider (e.g., assignment account) in Item #33, you must report the rendering/performing provider information in Item #24I and Item #24J. Enter the Rendering Provider’s NPI number in the non-shaded area of Item #24J. Note: In the case where a substitute provider (locum tenens) was used, the regular physician on whose behalf the services were furnished by a substitute is reported as the rendering provider. The HCPCS modifier Q6 is entered after the procedure code(s) in Item 24D to indicate that the services were provided by a substitute provider. When the Rendering Provider’s National Provider Identifier (NPI) is associated with more than one Highmark-assigned provider number, the Provider Taxonomy Code correlating to the contracted specialty must be submitted in addition to the NPI. This enables the accurate application of the provider’s contractual business arrangements with Highmark. In the shaded area of Item #24J, enter the Rendering Provider’s Taxonomy Code when required. |
|
|
25 |
Federal Tax ID Number |
Enter the federal tax ID (employer identification number) or Social Security number. Enter an X in the appropriate box to indicate which number is being reported. Only one box can be marked. This must be the tax ID which correlates to the billing provider reported in Item #33. |
|
|
26 |
Patient’s Account No. |
Optional. Highmark does not require this number for processing; however, we can reference this number when contacting your office for additional information. |
|
|
27 |
Accept Assignment? |
Enter an X in the correct box. Only one box can be marked. |
|
|
28 |
Total Charge |
Enter total charges for the services (i.e., total of all charges in column 24F). Enter amount right justified in the left-hand area of the field. Do not use commas or dollar signs when reporting dollar amounts. Do not report negative dollar amounts. |
|
|
29 |
Amount Paid |
Enter total amount the patient or other payers paid on the covered services only. Enter number right justified in the dollar area of the field. Do not use commas or dollar signs when reporting dollar amounts. Do not report negative dollar amounts. Enter 00 in the cents area if the amount is a whole number. |
|
|
30 |
Reserved For NUCC Use |
Highmark does not need this information to adjudicate the claim. Leave blank. |
|
|
31 |
Signature of Physician or |
This field must be completed on all claims to affirm that the reported services were performed by the provider, or performed under the provider's personal supervision. The name of the individual performing the service on the claim must be entered. The name may be computer printed or typed. Simply reporting the name of the group is insufficient. |
|
|
32 |
Service Facility |
Enter the name, address, city, state, and ZIP Code of the location where the services were rendered. The full nine digits of the ZIP+4 Code must be reported. Enter the 9-digit ZIP Code without the hyphen. The use of zeros (0000) or spaces for the last four digits of the ZIP+4 Code is not valid. Enter the name and address information in the following format: 1st Line – Name Note: A physical street address must be reported for the Service Facility Location — a P.O. Box or lock box will not be accepted. Highmark requires the Service Facility Location when the service was performed at a secondary location and the provider’s primary location was reported in Item #33. Highmark always requires the Service Facility Location when the Place of Service reported in Item #24B is one of the following: 21 – Inpatient Hospital |
|
|
32a |
Service Facility – NPI# |
Enter the NPI number of the service facility location. |
|
|
32b |
Service Facility – Other ID# |
When the National Provider Identifier (NPI) is associated with more than one Highmark-assigned provider number, the Provider Taxonomy Code correlating to the contracted specialty must be submitted in addition to the NPI. This enables the accurate application of the provider’s contractual business arrangements with Highmark. |
|
|
33 |
Billing Provider Info & PH # |
Item #33 identifies the provider that is requesting to be paid for the services rendered and should always be completed. Enter the billing provider's name, address, ZIP Code, and telephone number. The full nine digits of the ZIP+4 Code must be reported. Enter the 9-digit ZIP Code without the hyphen. The use of zeros (0000) or spaces for the last four digits of the ZIP+4 code is not valid. The telephone number is to be entered in the area to the right of the box title. Enter the name and address information in the following format: 1st Line – Name Note: A physical street address must be reported for the Billing Provider — a P.O. Box or lock box will not be accepted. |
|
|
33a |
Billing Provider - NPI# |
Enter the NPI number of the billing provider reported in Item #33. |
|
|
33b |
Billing Provider - Other ID# |
When the Billing Provider’s National Provider Identifier (NPI) is associated with more than one Highmark-assigned provider number, the Provider Taxonomy Code correlating to the contracted specialty must be submitted in addition to the NPI. This enables the accurate application of the provider’s contractual business arrangements with Highmark. Enter the PXC qualifier followed by the Provider’s Taxonomy Code when required. |
Additional Edit Checks for Paper Billers
Highmark does not attempt to correct or retrieve missing information for the situations listed below. Instead, these situations will result in a rejection of the claim, and you will be required to resubmit a new claim with the corrected data.
When a claim rejects, it is important for your billing staff and/or vendor to understand exactly what was wrong and what is needed to correct it.
If you submit paper claims, you may encounter the following denial codes and descriptions on your explanation of benefits notices:
|
Rejection Code |
Description |
|---|---|
|
B5606 |
In order to process the claim, additional information is required. Please resubmit the claim with a prescription for this service. Electronically enabled providers should resubmit electronically. |
|
P5039 |
In order to process this claim, additional information is required. The claim should be resubmitted with a valid modifier and associated number of services rendered. Electronically enabled providers should resubmit electronically. |
|
P5040 |
The patient’s coverage does not provide for this service in the place of treatment reported. Therefore, no payment can be made. |
|
P5010 |
The procedure code reported is not appropriate for the patient’s age. Please resubmit claim with verification of the patient’s age and/or a corrected procedure code. Electronically enabled providers should resubmit electronically. |
|
P5011 |
The procedure code reported is not appropriate for the patient’s age. Please resubmit claim with verification of the patient’s age and/or a corrected procedure code. Electronically enabled providers should resubmit electronically. |
|
P5012 |
The patient’s sex is invalid for the reported procedure. Please resubmit the claim with verification of the patient’s sex and/or a corrected procedure code or a complete description of service. Electronically enabled providers should resubmit electronically. |
The following entities, which serve the noted regions, are independent licensees of the Blue Cross Blue Shield Association: Western and Northeastern PA: Highmark Inc. d/b/a Highmark Blue Cross Blue Shield, Highmark Choice Company, Highmark Health Insurance Company, Highmark Coverage Advantage Inc., Highmark Benefits Group Inc., First Priority Health, First Priority Life, Highmark Care Benefits Inc., or Highmark Senior Health Company. Central and Southeastern PA: Highmark Inc. d/b/a Highmark Blue Shield, Highmark Benefits Group Inc., Highmark Health Insurance Company, Highmark Choice Company or Highmark Senior Health Company. Delaware: Highmark BCBSD Inc. d/b/a Highmark Blue Cross Blue Shield. West Virginia: Highmark West Virginia Inc. d/b/a Highmark Blue Cross Blue Shield, Highmark Health Insurance Company or Highmark Senior Solutions Company. Western NY: Highmark Western and Northeastern New York Inc. d/b/a Highmark Blue Cross Blue Shield. Northeastern NY: Highmark Western and Northeastern New York Inc. d/b/a Highmark Blue Shield.
All references to “Highmark” in this document are references to the Highmark company that is providing the member’s health benefits or health benefit administration and/or to one or more of its affiliated Blue companies.
All revisions to this Highmark Provider Manual (the “manual” or “Highmark Provider Manual”) are controlled electronically. All paper copies and screen prints are considered uncontrolled and should not be relied upon for any purpose.