Unit 4: Ancillary Services
4.4 West Virginia Senate Bill 273 - Alternative Treatments for Management of Chronic Pain
4.4 DME/Respiratory Supplies Management Program
4.4 Authorizing Durable Medical Equipment
4.4 Select DME Network (PA Only)
4.4 Billing For DMEPOS Provided to Members Registered as Inpatients or Outpatients at a Facility
4.4 Home Infusion Therapy Guidelines
4.4 DME Provided in a Physician's Office for Medicare Advantage (PA Only)
4.4 Medicare Advantage Guidelines for DMEPOS Upgrades (PA and WV Only)
4.4 Medicare Advantage Capped Rentals (PA and WV Only)
4.4 Medicare Advantage Home Oxygen Therapy (PA and WV Only)
4.4 Diabetic Testing Devices for Medicare Advantage Members (PA and WV Only)
Ancillary care refers to the wide range of health care services provided to support the work of physicians. To supplement the professional provider and facility networks, Highmark contracts with a network of ancillary providers that provide health care related equipment or services. These include freestanding and facility-based providers in specialties including, but not limited to:
- Durable medical equipment and supplies
- Orthotics/prosthetics
- Home infusion
- Ambulance
- Diagnostic services (radiology and laboratory)
- Therapeutic services (i.e., physical and occupational therapy, chiropractic services, and speech therapy)
In this Unit
This unit provides information and guidelines for providers of ancillary services such as durable medical equipment and supplies, orthotics, prosthetics, home infusion, therapy services, and more.
For diagnostic services, please see Chapter 4.5: Outpatient Radiology and Laboratory.
Network Participation
For information on applying to participate in Highmark’s facility and ancillary networks, please see Chapter 3.4: Organizational Provider Participation.
West Virginia Senate Bill 273 (the “Act”), effective June 7, 2018, was enacted in an effort to reduce opioid addiction by requiring health care insurers licensed in West Virginia to provide coverage for certain alternative treatments for management of chronic pain. The Act, in relevant part, amends Chapter 16 of the West Virginia Code relating to Public Health to add §16-54-1 et seq. (Treatment of Pain).
Requirements Under the Act
The following is a summary of the Act’s requirements:
- A health care practitioner can refer or prescribe any of the following treatment alternatives when a patient seeks treatment for chronic pain, based on their clinical judgment and the availability of the treatment, before starting a patient on an opioid: physical therapy, occupational therapy, acupuncture, massage therapy, osteopathic manipulation, chronic pain management program, and chiropractic services.
- All of these treatment alternatives do not need to be exhausted before prescribing an opioid.
- A practitioner may simultaneously prescribe an opioid along with any of the alternative treatments listed above.
- An insurer must provide, at a minimum, coverage for twenty (20) visits per event of physical therapy, occupational therapy, osteopathic manipulation, a chronic pain management program, and chiropractic services to treat conditions that cause chronic pain when ordered by a health care practitioner.
- A provider referral is not required as a condition of coverage for patients seeking these services.
- Any deductible, coinsurance, or copayment for these services may not be greater than the deductible, coinsurance, or copayment required for a primary care visit.
Applicability
Beginning with benefit plans renewing July 1, 2018, the Act will apply to Highmark West Virginia fully-insured large group and small group products, as well as Medicare supplemental group (Medifil) and individual (Medigap Blue) plans, upon renewal. The group products will continue to renew with the change through June 1, 2019.
Self-insured employer groups will be offered the opportunity to opt in and may or may not elect to follow the requirements of the Act.
The Act becomes effective on January 1, 2019, for individual Affordable Care Act (ACA) products, both on and off the Exchange.
Verify Benefits
To determine whether a member has coverage for alternative treatments for managing chronic pain as indicated under the Act, please be sure to verify the member’s benefits via Availity's Eligibility and Benefits Inquiry prior to providing services.
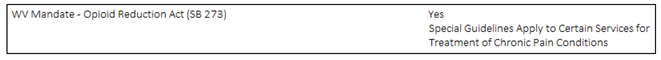
If the Act applies to a member’s benefit plan, it will indicate “Yes” for WV Mandate – Opioid Reduction Act (SB 273) under Product Wide Provisions. Benefit categories with special guidelines for visit limits per event for chronic pain include physical medicine, occupational therapy, and spinal manipulations.
Definitions
Chronic pain is defined as a non-malignant, non-end-of-life pain lasting more than three months or longer than the duration of normal tissue healing. Pain is considered chronic if it persists longer than expected after an illness or injury, if it is associated with a chronic pathological process, or if it flares up periodically over months to years.
Chronic pain may be caused by physical, psychological, and environmental factors. Chronic non-malignant pain encompasses many painful disorders including but not limited to back pain, migraine headaches, diabetic neuropathy, dental and orofacial pain, and arthritic pain.
An event is defined as an adverse or damaging medical occurrence resulting in an acute exacerbation of an existing chronic pain condition.
Chronic Pain Management Services
For following guidelines apply for chronic pain management services:
- The services must be provided in an outpatient setting, and
- The patient must have a diagnosis of chronic pain, and
- The patient must have an adverse or damaging medical occurrence resulting in an acute exacerbation of an existing chronic pain condition.
Applicable Diagnosis Codes
The Act applies to the following ICD-10-CM Primary Diagnosis Codes:
- G89.21 – Chronic pain due to trauma
- G89.28 – Other chronic post-procedural pain
- G89.29 – Other chronic pain
- G89.4 – Chronic pain syndrome
How Visit Limits Apply Per Event
The chronic pain visit limit per event is applied as a combination of physical therapy, occupational therapy, chiropractic services, osteopathic manipulation, and chronic pain management programs (and not as a visit limit per each service per event). Any combination of these services will fulfill the “per event” visit limit. In addition, the visit limits are combined for services provided in-network and out-of-network.
Note: Services received for diagnoses other than chronic pain will not apply to a member’s visit limit per event coverage for chronic pain. Please review the member’s benefits via Availity’s Eligibility and Benefits Inquiry for these services when they are provided for diagnoses other than chronic pain.
Highmark West Virginia Medical Policy
Please refer to the following Highmark West Virginia medical policies for physical and occupational therapy and manipulation services:
- Y-1 Physical Medicine
- Y-2 Occupational Therapy (OT)
- Y-9 Manipulation Services
In addition, please see Highmark West Virginia Medical Policy Y-23 Chronic Pain Management, effective September 17, 2018. This policy is applied on a post-payment basis and services will be subject to retrospective review.
Highmark West Virginia Medical Policy can be accessed under Policies & Programs from the main menu.
The purpose of this section is to provide Highmark’s guidelines for billing ground ambulance services for all commercial products. When used here, the term “ambulance transport services” includes all medically necessary ambulance services, except wheelchair van transport.
Medical Necessity
To be eligible for approval and payment, ambulance transport services must be medically necessary and appropriate. Medically necessary ambulance services are those rendered when the patient’s clinical condition is such that the use of any other method of transportation, such as a taxi, personal car, or other type of vehicle, would be contraindicated (e.g., it would endanger the member’s health).
Benefits
Although many Highmark benefit plans provide benefits for medically necessary ambulance transport services, benefits vary widely. The coverage available to any particular member is determined by the member’s specific benefit plan.
For medically necessary ambulance transport services provided to Highmark members, payment is made in accordance with the member’s benefit plan and, if applicable, the provider’s contract if the required benefit is available and the claim is billed appropriately.
Highmark’s determination on which entity is to bill for ambulance transport services is based on the Medicare program’s distinction between Part A and Part B services as in the table below. This standard applies to all Highmark products:
|
When the Medicare beneficiary is… |
The service falls under this program… AND |
Transportation is billed by… via this process… |
AND is reimbursed... |
|---|---|---|---|
|
An inpatient of a facility |
Medicare Part A |
The facility in which the beneficiary is an inpatient via the UB-04/837I claim |
As part of the DRG or per-diem payment for the inpatient stay |
|
Not an inpatient of a facility |
Medicare Part B |
The ambulance transport provider via the 1500/837P claim |
Via separate outpatient payment |
Emergent Situations
In the case of an emergency, any licensed ambulance transport provider (including a hospital-based service) may transport a Highmark member with coverage under any product from the scene of an accident or other initiating event to the closest facility that can provide the needed services.
- When the member is not an inpatient of any facility at the time of transport, the services must be billed to Highmark by the ambulance provider.
- If a member is an inpatient at one facility and is transported to another facility on an emergency basis, any licensed ambulance transport provider may transport the member. Unless the member is later returned to the original facility (which would typically be unusual in these circumstances), the member would not be considered an inpatient at the time. Therefore, the services must be billed to Highmark by the ambulance provider.
Assuming the member has coverage and the necessary benefit and that the claim is billed appropriately, payment will be made in accordance with the member’s benefit plan.
Non-Emergent Situations: To and From Hospitals
When a member must be transported from Hospital A to Hospital B, that member has been discharged from Hospital A. Since the member is no longer an inpatient at the time of transport, this service can be provided and billed by any licensed ambulance transport provider (including a hospital-based ambulance service). Assuming that the member has coverage and the necessary benefit and that the claims is billed appropriately, payment will be made in accordance with the member’s benefit plan and, if applicable, the provider’s Highmark contract.
Non-Emergent Inter-Hospital Transports with Return
If a member is transported from Hospital A to Hospital B to receive specialized services not available at Hospital A, and then returns to Hospital A, the member is considered an inpatient of Hospital A throughout the events, including the transport.
The ambulance transport services are part of Hospital A’s inpatient claim. The services can be provided by any licensed ambulance provider, which then must bill the hospital for the transport.
Under the Durable Medical Equipment (DME)/Respiratory Supplies Management Program, specific DME and supply items require authorization. Managed care plans typically require authorization -- PPO, EPO, HMO, IPA, POS, including Medicare Advantage PPO and HMO plans. However, benefits can vary and certain employer groups may choose to opt out of this requirement; always confirm DME authorization requirements under the member’s coverage. You can use the Availity® Eligibility and Benefits Inquiry transaction or the applicable HIPAA electronic transaction for benefit verification.
Highmark is responsible for claims processing, utilization management, and authorization functions for DME, prosthetics, orthotics, and supplies provided to Highmark members. Please verify benefits via Availity for a member’s specific coverage.
DME Requiring Authorization
Highmark maintains a List of Procedures/DME Requiring Authorization. This list is available on the Provider Resource Center under Claims & Authorization.
The authorization process for DME and supplies furnished through a stand-alone, Highmark participating ancillary DME suppliers for the items on the list is managed by Highmark’s Clinical Services. Ordering physicians may initiate authorization requests. Availity-enabled providers must submit the authorization request via Availity.
Important!
DME that does not require authorization simply requires a prescription written by the ordering physician.
Medicare Advantage
For Medicare Advantage members in Pennsylvania and West Virginia, all durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) claims that do not require authorization will process according to indications and limitations of Medicare Advantage Medical Policy. Items and services that are not considered to be medically necessary may not be billed to Medicare Advantage members without a Notice of Denial of Medical Coverage from Highmark (obtained through a preservice organization determination).
For information on preservice organization determinations for Medicare Advantage, please see Chapter 5.3: Medicare Advantage Procedures.
Claim Submission
Electronic claims submission is the preferred, most efficient, and most cost-effective method of submitting claims. If you are not yet submitting claims to Highmark electronically, visit the Electronic Data Interchange (EDI) Services website, which can be accessed from the Reimbursement Resources page on the Provider Resource Center. Or call EDI Operations toll-free at 800-992-0246, Monday through Friday, 8 a.m. to 4:30 p.m. EST.
You can also submit claims electronically through Availity's HIPAA-approved claims submission transaction. Once your claims are submitted to Highmark, whether through Availity or a HIPAA 837 electronic transaction, you are able to view the claim status and perform a Secure Message in Availity.
DMEPOS Refills
For all DMEPOS items that are provided on a recurring basis, suppliers are required to have contact with the member or caregiver/designee prior to dispensing refills. Highmark does not support or endorse auto-shipping; if the member is enrolled in or gives approval for auto-shipment of their supplies, the provider should not automatically ship the item(s). This is to ensure that the refilled item remains medically necessary, existing supplies are approaching exhaustion, and to confirm any changes/modifications to the order.
A refill request must be obtained from a member prior to delivery of any refill items. Refill requests are to be obtained on a monthly basis; refill requests for supplies should not extend beyond thirty (30) calendar days. The member’s refill request, including date of request and supplies requested, must be documented in the provider’s records and provided to Highmark upon request.
Documentation of Trial/Rental Period on CMN/LMN
If a Certificate of Medical Necessity (CMN) or Letter of Medical Necessity (LMN) indicates that a required trial/rental period for a DME item has occurred in the office, the provider must document the dates in which the trial occurred on the CMN/LMN.
If the dates of the in-office trial/rental are not indicated, the DME company is required to proceed as if the trial did not occur and must fulfill the trial/rental period prior to purchase.
The steps listed below describe the process to obtain authorization for durable medical equipment, prosthetics, orthotics, and respiratory supplies. Ordering physicians may initiate the authorization request.
This process applies to PPO, EPO, HMO, IPA, POS, and PPO Plus plans (including Medicare Advantage HMO and PPO plans in Pennsylvania and West Virginia).
Step 1: The requesting provider determines whether the request must be authorized by Highmark’s Clinical Services. Please gather all pertinent information, including a Certificate of Medical Necessity (CMN) if required, prior to submitting the request.
Step 2: If required, the requesting provider submits the request for authorization to Clinical Services through one of the following methods:
- If Availity-enabled, the request must be submitted via Availity.
- For those practices not yet Availity-enabled, fax an authorization request form to 412-544-2921 or 888-236-6321.
Step 3: Clinical Services will review the request.
- If benefits are not available, go to Step 4.
- If medical appropriateness cannot be determined, go to Step 5.
- If the request meets criteria, Clinical Services will approve the authorization request and notify the requester.
Step 4: If benefits are not available for the requested item or service, Clinical Services will deny the authorization request and notify the requesting provider.
A denial letter from Highmark will be sent to the ordering physician, vendor, and the member. Information regarding appeal/complaint rights will be detailed in the denial letter.
Step 5: If medical appropriateness cannot be determined from the documentation provided, Clinical Services will contact the requesting provider for additional information.
This information must be returned to Clinical Services in a timely manner, preferably within 48 hours, as regulatory time frames must be met.
Proceed to Step 6.
Step 6:
- If medical necessity cannot be determined, the authorization request is pended and sent to a Highmark physician reviewer for review. Proceed to Step 7.
- If the documentation substantiates the request, the service will be approved and the requesting provider will be notified.
Step 7: If the Highmark physician reviewer determines that the authorization:
Is medically appropriate…
Clinical Services will approve the pended authorization request and notify the requester.
Is not medically appropriate…
A physician will deny the pended request and send a denial letter to the ordering physician, vendor, and the member. A Clinical Services care manager will inform the requester of the denial.
To provide high-quality, cost-effective options to Highmark members in Pennsylvania, Highmark has contracted with certain durable medical equipment (DME) providers to form the Select DME Network. The more efficient, lower-cost network will provide a better value for Highmark members’ health care dollars.
Highmark has carefully evaluated and selected providers for the Select DME Network to ensure that all counties in Pennsylvania have adequate coverage to meet members’ needs. Additionally, there are several Select DME Network providers that provide DME on a national scale and are able to serve all counties in Pennsylvania.
Select DME Network Effective January 1, 2017
Effective January 1, 2017, the Select DME Network will be the exclusive network for all Highmark Medicare Advantage plans in Pennsylvania. For coverage of eligible DME services or supplies, Medicare Advantage members must obtain the services or supplies from a provider participating in the Select DME Network.
For Highmark commercial benefit plans, the Select DME Network applies to the highest tier level of Pennsylvania tiered health plans. For example, for a 3-tiered plan such as Connect Blue in western Pennsylvania, the Select DME Network applies to the Preferred tier level. In a two-tiered plan such as Community Blue Flex, Community Blue Premier Flex, and Alliance Flex Blue, the Select DME Network applies to the Enhanced tier level. Highmark commercial members with tiered plans have the option of choosing other DME participating providers not in the Select DME Network; however, receiving services or supplies from non-Select DME Network providers may result in higher out-of-pocket costs for members.
For More Information
Highmark provides two versions of the current list of providers in the Select DME Network. You can select a list of all participating providers or a list organized by category, which includes telephone numbers. These lists of providers in the Select DME Network are also available on the Provider Resource Center. Select Provider Network from the main menu, and then Select Durable Medical Equipment Network.
Select DME Network providers can be contacted directly if you have any questions about the products or services they provide.
Referring Highmark Members to DME Providers
Providers should refer their Highmark Medicare Advantage patients to Select DME Network providers for their DME equipment and supplies. Receiving services from non-Select DME Network providers would result in higher out-of-pocket costs for the member.
Highmark commercial members can continue to use providers from the broader DME network; however, you should refer Highmark commercial members to Select DME Network providers to receive the highest level of benefits possible.
Providers who supply durable medical equipment, orthotics, prosthetics, and supplies (DMEPOS) to Highmark members when they are registered as inpatients or outpatients at a Highmark-contracted facility may bill Highmark for a very limited scope of equipment and supplies.
Billing Guidelines
If a Highmark member is registered as an inpatient or outpatient of a hospital or skilled nursing facility (SNF), DMEPOS providers may bill Highmark for equipment or supplies provided to the member ONLY when one of the following apply:
- The equipment or supplies require approval and authorization by Highmark’s Clinical Services.
- The equipment or supplies are customized specifically for the individual member’s use in the home setting (e.g., customized power wheelchairs, customized splints or braces provided to the member for use in the home).
For any other DMEPOS supplies or equipment furnished to members who are registered as inpatients or outpatients of a facility, it is the responsibility of the Highmark-contracted hospital or SNF to provide the supplies or equipment and to seek payment from Highmark, as appropriate. Other DMEPOS supplies or equipment include, but are not limited to, items such as crutches, walkers, canes, and soft goods.
These requirements apply to all Highmark products, including Medicare Advantage HMO and PPO products available in Pennsylvania.
Exceptions for Medicare Advantage Members Residing in SNFS
These requirements do not apply in the case of DMEPOS items provided to Medicare Advantage HMO or PPO members residing in a SNF who have exhausted their 100-day skilled nursing benefit or are receiving a non-skilled level of care.
Under these circumstances, the billing process should be treated as if the member is living in his or her own residence. Therefore, the DMEPOS provider would bill the claim to Highmark.
Home infusion therapy (HIT) is the administration of medically necessary fluids or drugs through a central line or peripheral vein to Highmark members in their homes or places of residence.
Drug therapies commonly administered by infusion include antibiotics, chemotherapy, pain management, and parenteral nutrition.
Here are examples of certain conditions that commonly require infusion therapy:
- Infections that are unresponsive to oral antibiotics
- Cancer and cancer-related pain
- Gastrointestinal diseases or disorders that prevent normal functioning of the gastrointestinal system
- Immune disorders
Home nursing services are also provided to ensure proper patient education and training and to monitor the care of the patient in the home.
Provider Guidelines
Home infusion therapy providers must possess a current pharmacy license from the state in which they provide services. They must also maintain accreditation from one of the following: The Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations); Accreditation Commission for Health Care, Inc.; Community Health Accreditation Program, Inc.; The Compliance Team, Inc.; or Healthcare Quality Association on Accreditation.
Provider agrees to submit claims to Highmark for all Highmark members (must use best efforts to submit claims electronically). Providers also agree to accept Highmark’s payment for covered services they perform. The provider will not charge the member for covered services the provider has agreed to provide except for applicable copayment, coinsurance, and deductible amounts.
In Pennsylvania, the provider agrees to provide:
- Dedicated customer service personnel
- A toll-free telephone number
- Twenty-four hour availability for service and delivery
- Twenty-four hour turnaround time to accept patient to service except for customized, specialized, or significantly customer-specific product
Nursing Services for Home Infusion Therapy
Per diem rates are all-inclusive rates for medically necessary services. They include all ancillary services and supplies (e.g., durable medical equipment or supplies as needed, educational materials, basic solutions, administrative supplies, and the defined nursing hour increment).
Daily maintenance and a flush kit are integral components to the per diem allowance regardless of the mode of access. Since daily maintenance and flush kits were considered in the development of the fee schedule, Highmark will not provide separate payment for these services.
Multiple Infusion Therapies
Multiple infusion therapies apply to patients who require multiple concurrent infusion treatments including, but not limited to, multiple antibiotics, hydration, chemotherapy, and enteral feeding therapy. Highmark will not reimburse separately for each therapy. Instead, the provider must bill and will be reimbursed for the most costly per diem that applies plus the drug(s) administered.
When billing for multiple therapies on the same claim, bill only for the most costly procedure. Do not report zero dollar charges for the remaining therapies.
Exception: The only exception to this is aerosolized AIDS drug therapy. It is the only therapy that must be billed in conjunction with another mode of home IV therapy administration. It is also the only drug therapy that, while provided as part of a multiple-therapy treatment, can be billed as a separate service. Use procedure code S9061 to report aerosolized AIDS drug therapy.
Billing and Reimbursement for Drugs Administered
Follow these guidelines when reporting drugs administered by home infusion therapy:
- If the patient administers the drugs, and the home infusion provider provides the drugs but no nursing services, bill for the supplies or drugs but not a per diem nursing visit.
- Report the correct procedure code according to the date of service and the effective date of your contract.
- When billing for drugs administered through home therapy infusion, bill the amount of drug based on the smallest available commercial size.
- Drug claims billed under Highmark medical benefits require the submission of National Drug Code (NDC) information. Please see the List of Procedures Requiring NDC Information. This list is also available under Policies & Programs then Pharmacy Programs on the Provider Resource Center.
Highmark has always maintained a list of durable medical equipment (DME), prosthetics, orthotics, and supplies incidental to a physician or facility that can be furnished to members for their convenience in the physician office setting. This list applies only to Medicare Advantage products with DME benefits.
The list includes minor DME items, prosthetics, orthotics, and supplies incidental to a physician or facility that can be furnished to members for their convenience in the physician office setting.
These items do not require authorization and can be billed to Highmark for reimbursement at fee-for-service. Member cost-sharing may apply.
Physician Office DME Supply List for Medicare Advantage
For the complete list of DME, prosthetics, orthotics, and supplies that can be provided to Medicare Advantage members in the physician’s office, click here.
Note: For items not on this list, please direct members with Medicare Advantage HMO and Freedom Blue PPO to a participating network vendor.
Important! Always Verify Benefits
Please verify the member’s benefits through Availity® prior to providing any of these items. Member cost-sharing in the form of deductible or coinsurance may apply to DME and supplies under the member’s Medicare Advantage plan.
Generally, upgrades to durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) are defined as items that go beyond what is medically necessary. An upgrade may be from one Healthcare Common Procedure Coding System (HCPCS) code to another HCPCS code, or it may be from one item to another within the same HCPCS.
The payment for an item must be consistent with what is considered reasonable and medically necessary to serve the intended purpose. In cases where an item is considered to be medically necessary and covered, and a member wishes to obtain an item with upgraded features, payment is based on the allowance for the item normally used for the intended purpose.
Claim Submission and Reimbursement
Highmark requires providers to bill these services as they do for Medicare fee-for-service beneficiaries. The items should be billed as two (2) separate line items, one for the upgraded item and one for the standard item.
If it is determined that the upgrade was not medically necessary, payment is made on the standard item and the line item for the upgraded item will be denied. Liability will be set based on which modifiers were billed on the line.
Highmark adopted the Centers for Medicare & Medicaid Services (CMS) payment methodology on capped rental items for all Medicare Advantage products. These items are denoted as payment class “CR” (Capped Rental) on the Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) fee schedule.
Under the CMS payment methodology, items denoted as payment class CR are paid for as rentals only. Generally, they cannot be purchased upfront, except in certain situations (e.g., electric wheelchairs meeting certain criteria). Upon reaching the final monthly payment on items and services in this category, ownership will transfer to the member.
Note: Claims for rental items not designated as CR will continue to be paid at the monthly allowable fee until the purchase price is met at which time ownership of the item will transfer to the Highmark patient.
Payment Methodology and Required Modifiers for Capped Rentals
The following chart outlines the payment schedule and required modifiers for capped rental items for Medicare Advantage:
|
Schedule |
Payment |
Required Modifier |
|---|---|---|
|
Month 1 |
10% of purchase price paid |
KH |
|
Months 2-3 |
10% of purchase price paid |
KI |
|
Months 4-13 |
7.5% of purchase price paid |
KJ |
Exception: Power wheelchairs pay at 15% for months 1-3 and 6% for months 4-13. Modifiers are the same as above.
List Of Capped Rental Items
For a complete list of procedure codes for DMEPOS items that fall into this capped rental classification, click here.
Medicare Advantage HMO and PPO products provide coverage for medically necessary home oxygen therapy and the equipment necessary for the safe, effective delivery of that therapy.
Oxygen Equipment Limited to 36-Month Rental Period
Reimbursement for oxygen equipment is limited to 36 monthly rental payments to mirror the Centers for Medicare & Medicaid (CMS) payment methodology.
Payment for accessories (e.g., cannula, tubing, etc.), delivery, back-up equipment, maintenance, and repairs will be included in the rental allowance. Payment for oxygen contents (stationary and/or portable) will also be included in the allowance for stationary equipment (E0424, E0439, E1390, E1391).
After the 36-month rental period ends, according to CMS policy, Highmark will pay for oxygen contents monthly and for maintenance once every six months. Ownership of the oxygen delivery equipment will remain with the equipment supplier.
Supplier Responsibilities
The supplier who provides oxygen equipment for the first month must continue to provide any necessary oxygen equipment, and all related items and services, through the 36-month rental period unless one of the following exceptions is met:
- The beneficiary relocates temporarily or permanently outside of the supplier’s service area;
- The beneficiary elects to obtain oxygen from a different supplier; or
- Highmark makes individual case exceptions.
Providing different oxygen equipment/modalities (e.g., concentrator [stationary or portable], gaseous, liquid, transfilling equipment) is not permitted unless one of the following requirements is met:
- The supplier replaces the equipment with the same or equivalent item;
- The physician orders different equipment;
- The member chooses to receive an upgrade and signs a Pre-Service Denial Notice; or
- Highmark determines that a change in equipment is warranted.
Reasonable Useful Lifetime (RUL)
After 36 rental payments have been made, there will be no further payment for oxygen equipment during the 5-year reasonable useful lifetime (RUL) of the equipment. The RUL is not based on the chronological age of the equipment. It starts on the initial date of service and runs for five years from that date.
If use of portable equipment (E0431, E0433, E0434, E1392, K0738) begins after the use of stationary equipment begins, payment for the portable equipment can continue after payment for the stationary equipment ends until 36 rental payments have been made for the portable equipment.
The supplier who provided the equipment during the thirty-sixth rental month is required to continue to provide the equipment, accessories, contents (if applicable), maintenance, and repair of the oxygen equipment during the 5-year RUL of the equipment.
Any time after the end of the 5-year RUL period for oxygen equipment, the beneficiary may elect to receive new equipment, thus beginning a new 36-month rental period.
Payment for Oxygen Content
Payment for stationary and portable contents is included in the fee schedule allowance for stationary equipment. No payment can be made for oxygen contents in a month in which payment is made for stationary equipment.
If the patient was using stationary gaseous or liquid oxygen equipment during the thirty-sixth rental month, payment for stationary contents (E0441 or E0442) begins when the rental period for the stationary equipment ends.
Conditions for Which Coverage is Available
Home oxygen therapy coverage is available for rented, not purchased, oxygen equipment for members with significant hypoxemia in the chronic stable state provided all of the following conditions are met:
- The attending or consulting physician has determined that the patient suffers a severe lung disease or hypoxia-related symptoms that might be expected to improve with oxygen therapy.
- The patient’s blood gas levels indicate the need for oxygen therapy.
- Alternative treatment measures have been tried or considered and have been deemed clinically ineffective.
Conditions for Which Coverage is Not Available
Coverage for oxygen therapy for Medicare Advantage members is not available for the following conditions:
- Angina pectoris in the absence of hypoxemia. This condition is generally not the result of a low oxygen level in the blood, and there are other preferred treatments.
- Dyspnea without cor pulmonale or evidence of hypoxemia.
- Severe peripheral vascular disease resulting in clinically evident desaturation in one or more extremities. There is no evidence that increased PO2 will improve the oxygenation of tissues with impaired circulation.
- Terminal illnesses that do not affect the respiratory system.
Portable Oxygen Systems
Coverage of a portable oxygen system alone or to complement a stationary oxygen system may be allowed if the patient is mobile within the home. When submitting an authorization request, please check both the “portable” box and the “stationary” box.
Spare Tanks Or Emergency Inhalators
Spare tanks of oxygen or emergency oxygen inhalators are considered not medically necessary since these items are precautionary and not therapeutic in nature.
Blood Oxygen Determinations
Initial orders for oxygen therapy must also include the results of a blood gas study, usually a measurement of the partial pressure of oxygen (PO2) in arterial blood. The study must be performed within 30 days before the date of service.
The study should be performed under one of the following circumstances:
- Ordered and evaluated by the attending or consulting physician.
- Ordered and evaluated by the attending physician and performed under his or her supervision.
- Performed by a qualified provider of laboratory services.
Note: Highmark does not consider suppliers as qualified to perform blood gas studies and will not pay for a qualifying blood gas study if performed by a supplier.
Conditions of Blood Gas Studies
The conditions under which the blood gas study was performed must be specified in writing and submitted on the Certificate of Medical Necessity (CMN) form. Examples of this documentation may include: at rest, while sleeping, while exercising, on room air, on oxygen, etc.
Note: If the study is performed while the patient is receiving oxygen, indicate the amount, body position during testing, and any additional information required for interpretation.
Blood Gas Level Criteria
The table below describes three groups of blood gas levels for which coverage is provided.
|
Group |
Blood Gas Level Criteria |
|---|---|
|
GROUP 1: Medically necessary |
Arterial PO2 is at or below 55 mm Hg, or arterial oxygen saturation is at or below 88% taken at rest. OR Arterial PO2 is at or below 55 mm Hg, or arterial oxygen saturation is at or below 88% taken during sleep for a patient who demonstrates arterial PO2 at or above 56 mm Hg or arterial oxygen saturation at or above 89% while awake. OR A greater than normal fall in oxygen level during sleep (arterial PO2 decreases more than 10 mm Hg, or arterial oxygen saturation decreases more than 5%) associated with symptoms or signs reasonably attributable to hypoxemia (e.g., cor pulmonale, “P” pulmonale on EKG, documented pulmonary hypertension, and erythrocytosis). OR Arterial PO2 is at or below 55 mm Hg or arterial oxygen saturation at or below 88%, taken during activity for a patient who demonstrates arterial PO2 at or above 56 mm Hg or arterial oxygen saturation at or above 89%, during the day while at rest. In this case, supplemental oxygen is provided during exercise if it is documented that the use of oxygen improves the hypoxemia that was demonstrated during exercise when the patient was breathing room air. |
|
GROUP 2: Medically necessary |
Arterial PO2 is 56 to 59 mm Hg or arterial blood oxygen saturation is 89% if any of the following are documented:
|
|
GROUP 3: Not medically necessary |
Home use of oxygen is not medically necessary for members with PO2 levels at or above 60 mm Hg, or arterial blood oxygen saturation at or above 90%. |
Additional Studies
Retesting between the 61st and 90th day of home oxygen therapy is required in order to establish continued medical necessity when a patient’s initial certification for oxygen is approved based on one of the following criteria:
- Arterial PO2 was 56 mm Hg or greater
- Oxygen saturation was 89% or greater
Certificate Of Medical Necessity (CMN)
A Certificate of Medical Necessity (CMN) form for home oxygen is necessary for the following:
- Initial certification
- Recertification
- Changes in the oxygen prescription
The CMN must be completed, signed, and dated by the ordering physician.
Obtaining Authorization
Please review the prior authorization list on the Provider Resource Center for your region to determine which oxygen services require an authorization. If authorization is required, follow the steps listed below:
|
STEP |
ACTION |
|---|---|
|
1 |
If Availity-enabled, the vendor or physician must enter an authorization request for oxygen into Availity. A Certificate of Medical Necessity (CMN) must be completed for the situations indicated above. If not Availity-enabled, the vendor or physician should fax a CMN form to Clinical Services at 412-544-2921 or 888-236-6321. |
|
2 |
If a required CMN form has not been submitted, Clinical Services will contact the provider and request that one be completed. |
|
3 |
Once all information has been received, the DMEPOS authorization process will be followed (as detailed on earlier in this unit). |
Recertification
Recertification must include the results of a recently performed arterial blood gas (ABG) or oximetry test; and it is required one to three months after initial certification under the following circumstances:
- If the patient’s arterial PO2 was 56 mm HG or greater at the initial certification.
- If the patient’s oxygen saturation was 89% or greater at the initial certification.
- If the physician initially estimated that oxygen was needed for one to three months.
Note: Once recertification establishes medical necessity for continued therapy, subsequent recertification is not required except when there is a change in the oxygen prescription or the attending physician.
Medicare Advantage HMO and PPO products provide coverage for medically necessary diabetic testing devices including glucometers, test strips, and lancets under the durable medical equipment (DME) benefit. Insulin pens and insulin pumps are also covered under the DME benefit.
Insulin and syringes will not be covered as DME, but will be covered under the Medicare Part D Prescription Drug Benefit.
Purchasing Diabetic Testing Devices
Members are able to purchase diabetic testing devices from any participating, in-network DME vendor with applicable member cost-sharing under Medicare Advantage. Supplies obtained from an in-network DME supplier are covered in full after coinsurance.
Although Medicare Advantage PPO members have out-of-network benefits, those members who elect to go out-of-network to purchase DME supplies will incur additional out-of-pocket expenses. Please review the patient’s specific benefit design to determine possible authorization requirements and/or coinsurance amounts and maximum annual coinsurance amounts.
Prescriptions for Multiple, Daily Diabetic Testing
If a patient is instructed to test multiple times in the same day for diabetes, treatment prescriptions for DME diabetic supplies should be written clearly to state the correct frequency of testing (e.g., “to be tested three times daily”). This will ensure that the correct amount of supplies are ordered and submitted for DME coverage under a Medicare Advantage product.
Many of the in-network DME vendors can supply increased supplies in a timely manner. If a patient requires additional supplies, the treating physician will need to provide the patient with a new prescription detailing the testing frequency. After receiving the new prescription, the patient will need to contact the DME vendor to indicate that their testing needs have increased and that their physician wrote a new prescription detailing the change.
Mail-Order Diabetic Testing Supplies
Members are able to order 90-day supplies of diabetic supplies via mail order. The physician must write the prescription to reflect the long-term supply so that the member is able to submit the prescription to the mail order DME vendor and receive accurate long-term supplies.
For More Information
If you have specific questions about diabetic testing devices for Medicare Advantage members, please contact the Provider Service Center.
The following entities, which serve the noted regions, are independent licensees of the Blue Cross Blue Shield Association: Western and Northeastern PA: Highmark Inc. d/b/a Highmark Blue Cross Blue Shield, Highmark Choice Company, Highmark Health Insurance Company, Highmark Coverage Advantage Inc., Highmark Benefits Group Inc., First Priority Health, First Priority Life, Highmark Care Benefits Inc., or Highmark Senior Health Company. Central and Southeastern PA: Highmark Inc. d/b/a Highmark Blue Shield, Highmark Benefits Group Inc., Highmark Health Insurance Company, Highmark Choice Company or Highmark Senior Health Company. Delaware: Highmark BCBSD Inc. d/b/a Highmark Blue Cross Blue Shield. West Virginia: Highmark West Virginia Inc. d/b/a Highmark Blue Cross Blue Shield, Highmark Health Insurance Company or Highmark Senior Solutions Company. Western NY: Highmark Western and Northeastern New York Inc. d/b/a Highmark Blue Cross Blue Shield. Northeastern NY: Highmark Western and Northeastern New York Inc. d/b/a Highmark Blue Shield.
All references to “Highmark” in this document are references to the Highmark company that is providing the member’s health benefits or health benefit administration and/or to one or more of its affiliated Blue companies.
All revisions to this Highmark Provider Manual (the “manual” or “Highmark Provider Manual”) are controlled electronically. All paper copies and screen prints are considered uncontrolled and should not be relied upon for any purpose.