Unit 3: Professional Provider Guidelines
Highmark is committed to ensuring that the information in the Highmark Provider Directory meets Centers for Medicare & Medicaid Services (CMS) regulations and National Committee for Quality Assurance (NCQA) standards, as well as our own standards of quality.
In addition, Highmark members use the Highmark Provider Directory to make informed decisions when selecting a provider; therefore, it is also crucial to your practice to ensure your information is always accurate and up-to-date for the Provider Directory.
CMS Requirements
CMS requires Highmark to have the most current information on our network providers and requires ongoing review of all physician information listed in the Provider Directory to confirm:
- The provider’s name is correct.
- The practice name is correct.
- The provider’s practicing specialties are correctly listed.
- Providers are not listed at practice locations where they do not actually accept appointments and see patients.
- The provider is accepting new patients, or not accepting new patients, at the location.
- The provider’s street address and phone number are correct.
NCQA Requirements
NCQA also requires the Provider Directory to include, and Highmark to confirm, the same physician information as listed above for CMS, as well as the physician’s hospital affiliation. Hospital affiliation means the hospital(s) in Highmark’s networks where physicians have admitting or attending privileges.
Policy
Providers are required to review and update their information as soon as a change occurs. All data should be reviewed once a quarter, at a minimum, to ensure accuracy. Providers who do not verify or update their data in a timely manner will be removed from the Highmark Provider Directory. In addition, your status within Highmark’s networks may be impacted.
Provider Data Maintenance & Provider File Management
You may review your detailed, real-time billing provider information in Provider Data Maintenance or Provider File Management (Delaware, Pennsylvania, and West Virginia only) in Availity. Once you log into Availity, go to Payer Spaces and then select Provider Data Maintenance or Provider File Management (Delaware, Pennsylvania, and West Virginia only).
Please see the section of this unit on Reporting Changes in Your Practice for additional information on reviewing your information and instructions for making necessary changes via Availity or forms, if necessary.
Network providers are required to maintain current, detailed, comprehensive, and accurate medical records for each member to whom they provide services. The medical record is critical to ensuring the quality, coordination, and continuity of care.
Each record must support the service billed and the level of care provided on each unique date. Records that contain cloned documentation, conflicting information, or other such irregularities may be disallowed for reimbursement. Reimbursement for any record containing such questioned documentation will be represented in overpayment calculations with zero reimbursement allowed.
Standards of Documentation
Each medical record should contain:
- Biological, demographic, and other personally identifying information for the member;
- Patient-identifying information on each page to ensure pages are not lost or misfiled;
- Identification of the treating provider and the services he/she provided on each entry;
- Date of each provider/patient encounter and date of each entry;
- Information on allergies and adverse reactions or, if none, notation that the patient has no known allergies or history of adverse reactions;
- Prescribed medications, including dosages and dates of initial or refill prescriptions;
- Problem list, including significant illnesses and medical and psychological conditions;
- Presenting complaints, working diagnoses, and treatment plans;
- History and physical examination for each encounter appropriate to the reason for the particular encounter;
- Past medical history, examinations, treatments, social history, and risk factors pertinent to developing a treatment plan;
- Documentation that laboratory tests, other studies ordered, and consultations are appropriate to the member’s symptoms or condition, and that results have been reviewed and acted upon;
- Documentation of required follow-up, including any diagnostic testing, treatment, or education;
- Documentation that information received from another provider has been reviewed and, where appropriate, acted upon;
- Tracking and review of problems from previous visits, including management of chronic conditions;
- Documentation sufficient to demonstrate the medical necessity and appropriateness of each service;
- Copies of advance directives or documentation of discussions with adult patients about such directives;
- Immunization records (for PCPs);
- Documentation of tobacco or alcohol use, or substance abuse;
- Documentation of member input into treatment plans and decisions;
- Preventive services, referrals, or counseling, where appropriate;
- Copies of consents or releases, where required, for release of confidential health information; and
- Legible entries.
Note: These standards have been approved by the Highmark Credentialing Committees, the voting members of which are practicing physicians in the applicable Highmark networks.
Important! Signature Required
All entries in the record must contain a valid, legible author’s signature, which may be a handwritten signature with credentials, printed name and credentials accompanied by handwritten provider initials, or unique electronic identifier with credentials.
Maintenance of Records
Medical records must be maintained in accordance with the following requirements:
- Each chart is labeled to allow for easy and timely retrieval by the provider or provider’s staff to meet the patient’s clinical needs;
- Records are systematically and timely prepared, filed, and stored; and
- Safeguards are in place to protect the confidentiality of patient records and information.
Monitoring Compliance
Highmark will monitor compliance with medical record documentation and maintenance standards in a number of ways. These may include: site visits in connection with credentialing, collection of HEDIS or other data; or monitoring compliance with contract, regulatory, or accreditation requirements; review of records in connection with billing audits or other provider monitoring activities; review of records in connection with investigation of quality of care concerns; investigation of complaints; and as part of quality improvement initiatives.
Providers whose records are not in compliance may be subject to written counseling, corrective action including repayments and follow-up reviews.
Highmark periodically engages in the review of members’ medical records as well as inspection of network providers’ offices. Highmark reviews medical records for a number of reasons pertaining to the administration of high-quality managed care benefit programs. The reasons include, but are not limited to:
- To evaluate the appropriateness of billing or level of utilization of services
- To determine the medical necessity and appropriateness of a claim when we have insufficient information
- For credentialing and recredentialing network providers (does NOT apply to Pennsylvania’s Participating Provider Network)
- To evaluate the clinical quality of care provided to members
- To determine possible pre-existing conditions
- For conducting condition management for the benefit of members
- To investigate complaints
- For verifying immunization of pediatric and adult patients
- For risk adjustments
- For appeals and audits
Medical Records Requests
Network providers are required to cooperate with and timely respond to requests for medical records from Highmark. Regulatory standards require health plans to make medical necessity determinations, request and review additional information, and process claims within strict time frames. For this reason, it is important for providers to provide all relevant medical records within the time frame stipulated in the written request. No response or a late response may result in a denial of payment.
Clinical quality of care issues are reviewed by the plan’s clinical staff and, if necessary, a medical director. Failure to provide records requested may result in disciplinary action, up to and including termination from Highmark network participation.
Billing reviews may determine whether services billed are documented and supported by the medical record. Highmark reimburses only for medically necessary covered services. Failure to furnish requested medical records may result in Highmark recouping prior payments.
Highmark’s procedures for requesting and using medical records are designed to avoid multiple requests for the same records, request only the minimum necessary records, and protect the confidentiality of information and the privacy of individuals.
Network providers are not reimbursed for supplying requested medical records to Highmark.
Member Consent
As a HIPAA covered entity, Highmark has established as its policy that we will not request or obtain consent of our members in connection with the use or disclosure of protected health information (PHI) for treatment, payment, or health care operations. Highmark has received a general consent from our members. Each member completes and signs an enrollment form that provides for the release of most information relating to past, present, or future health care examinations or treatments for anyone covered under the enrollment form. Such consent is necessarily broad to enable Highmark to administer high-quality benefit programs.
Information collected is handled with a high level of security and respect for privacy. However, member records that include information relating to behavioral health, human immunosuppressant virus (HIV), Acquired Immune Deficiency Syndrome (AIDS), sexually transmitted diseases (STDs), and/or substance abuse could be subject to extra protections regarding disclosure under state laws. In such cases, providers asked to submit medical records are responsible for obtaining member consent and should submit it to Highmark along with the requested documents, as payment for services provided are specifically conditioned upon receipt of supporting documentation.
Alternatively, providers may choose to delete the personally identifying details from those records containing any such protected information prior to submitting the medical records to Highmark for review.
Provider Cooperation
The terms of the network agreement require the full cooperation of network providers with all office reviews. Failure to supply requested copies of medical records or failure to cooperate with office inspections of medical records may result in termination from Highmark network participation.
Highmark requires all physicians who provide services to our members to be credentialed and contracted. However, under certain circumstances, Highmark allows for locum tenens arrangements.
A locum tenens, or “substitute physician,” is defined as a practitioner who is covering for another physician when they are absent for reasons of illness, medical leave, vacation, military leave, or continuing medical education, or in the event of a practitioner’s retirement or death.
Service Time Frame
Locum tenens service time frames may not exceed 60 consecutive days for Medicare Advantage or Commercial networks.
If a regular physician is absent longer than 60 days without returning to work and is covered by one locum tenens, the locum tenens must be credentialed and enrolled as if he or she were joining your practice as a new physician. It is recommended that the credentialing process be started as soon as possible to help reduce any gaps in services.
For credentialing requirements, please see Chapter 3 Unit 2: Professional Provider Credentialing.
Requirements
Highmark does not enumerate substitute physicians. A physician may bill and receive payment for the substitute physician’s covered services as though he/she performed them. With respect to physicians, the term “covered visit service” includes not only those services ordinarily characterized as a covered physician visit but also any other covered items and services furnished by the substitute physician or by others as “incident to” the physician’s services.
A physician may submit a claim and, if assignment is accepted, receive payment for covered visit services of a substitute physician if:
- The regular physician is unavailable to provide the services;
- The member has arranged or seeks to receive the services from the regular physician;
- The regular physician pays the substitute physician for his/her services on a per diem or similar fee-for-time basis;
- The substitute physician does not provide the services to members over a continuous period of longer than 60 days. Exception: If the regular physician is called to active duty in the Armed Forces, services provided by a substitute physician may be billed under a fee-for-time compensation arrangement for longer than the 60-day limit; and
- The regular physician indicates on the claim that the services were provided by a substitute physician under a fee-for-service compensation arrangement by including the Q6 Modifier, which designates services were performed by a substitute physician.
Note: If the only services a physician performs in connection with an operation are post-operative services furnished during the period covered by the global fee, these services would not be identified on the claim as services furnished by a substitute physician.
Billing Guidelines
Claims for the services of a substitute physician are billed as though the regular physician performed the services; the regular physician on whose behalf the services were furnished by a substitute is identified as the rendering provider on the claims (Item 24J on the 1500).
To receive payment for a substitute physician’s covered services, the regular physician must include the Q6 modifier after the procedure code(s) (Item 24D on the 1500).
A record of each service provided by the substitute physician must be kept on file along with the substitute physician’s NPI. This record must be made available to Highmark upon request. Claims submitted with a Q6 modifier will be subject to ongoing monitoring and auditing.
Highmark allows participating providers to request copies of their participating physician contract, as required. Highmark will provide a copy of the contract with participating physicians, including certain contracts with physician organizations or physician groups where participating physicians participate. Highmark is restricted, however, to provide contracts to requesters if the terms of the contract restrict the request.
How to Request a Copy of Your Contract
Professional providers can request a copy of their contract by submitting the Request to be a Highmark Professional Participating Provider form. Organizational providers may mail a written request for a copy of their contract to:
| Highmark Provider Information Management P.O. Box 898842 Camp Hill, PA 17089-8842 |
Upon receipt of the request, Highmark’s Provider Information Management will provide the requestor with one copy of their participating physician contract, unless otherwise requested. Requests generally take 15 business days to process. Please allow ample time for processing before checking the request status.
Policy for Changing Practice Information
The provider database maintained by Highmark contains vital information regarding each network practitioner. By keeping your practice information updated, you help Highmark do the following:
- Maintain compliance with federal regulations and National Committee for Quality Assurance (NCQA) standards
- Process claims correctly
- Notify members of the names and addresses of network practitioners
- Notify primary care practitioners of available specialists to whom they may refer
Most changes will require Highmark to revise existing provider files. In most cases, membership or claims payment will be affected by changes in your practice. Therefore, if you do not give advance notification, we cannot guarantee accurate membership information, claims, and/or claims payments. Certain changes may necessitate the issuance of a new contract.
Note: Your up-to-date information must include your current address, phone number, email address, and fax number, and any and all required data elements set forth in your provider contract(s) with Highmark.
Highmark will primarily communicate with you via email regarding your credentialing. Please ensure your email address on file is current and accurate.
Type of Changes to Report
The following is a list of changes in your practice that must be communicated to Highmark:
- Practice location change
- Billing/mailing address change
- Telephone number change
- Fax number change
- Hospital affiliation change
- Medical group affiliation change
- Office hours change
- New tax identification number
- Practice name change
- Practitioners joining the practice
- Practitioners leaving the practice (including through retirement or death)
- Changes in malpractice insurance coverage levels (10 days in advance of any reduction or termination of coverage)
- Practice mergers
- Practice acquisitions
- Addition or closure of a practice site
- Changes in acceptance of new patients
- Changes in practice locations where practitioners see and treat patients
- Languages spoken by the physician or clinical staff
- Board certification change
- Specialty change
Using Availity Essentials® to Report Updated Practice Information
All Availity-enabled practitioners should make their practice information changes via Provider Data Maintenance or Provider File Management (Delaware, Pennsylvania, and West Virginia only) in Highmark's Payer Spaces in Availity. This function can be used to update the practice information such as contact information, practitioners affiliated with a location, office hours, age range the practice serves, etc.
Once in Payer Spaces, click Provider Data Maintenance or Provider File Management (Delaware, Pennsylvania, and West Virginia only), and then select the location for which updates are needed. Click on the Edit button next to the information that requires change.
Detailed instructions are available in the Provider Data Maintenance Guide and the Provider File Management Guide (Delaware, Pennsylvania, and West Virginia only). The guides are available on the Provider Resource Center under Resources & Education, then Provider Data Accuracy Compliance.
How to Use Availity to Add or Delete Practitioners
Availity-enabled practices can use Provider Data Maintenance or Provider File Management (Delaware, Pennsylvania, and West Virginia only) to add practitioners or remove practitioners from their assignment accounts.
The addition of an individual practitioner to a group or the deletion of an individual practitioner from the group, via this real-time function, requires only one electronic signature. The Authorized Representative of the Group is able to complete both additions and deletions. If a new practitioner has never completed an Initial Credentialing Application with Highmark, they must do so before being added to your group.
Note: Your Availity Security Officer can generate a username for a practitioner new to your assignment account.
How to Update Practice Information for Non-Availity Enabled Practitioners
Practitioners who are not Availity-enabled must notify Highmark of any change to their practices. The Addition Request to Existing Assignment Account form can be completed electronically for practitioner changes.
For additional practice addresses or for address changes, complete the Provider Directory Update Form.
These forms can be accessed on the Provider Resource Center – under Resources & Education in the main menu select Forms, and then Provider Information Management Forms.
Important!
All practitioners joining or leaving an established practice or leaving a Highmark network must notify Highmark 60 days before the event.
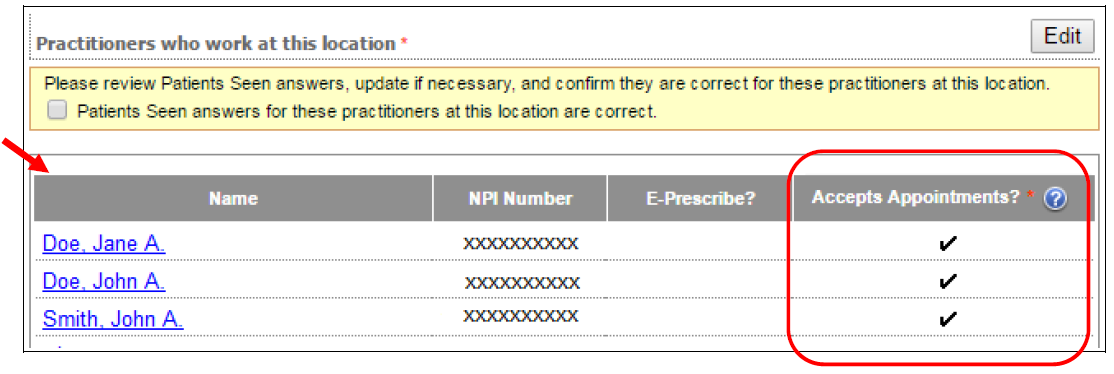
Updating “Accepts Appointments?”
The “Accepts Appointments?” question requires a response in Provider File Management, which is available in Payer Spaces in Availity. When adding a new practice address, affiliating a new practitioner to an existing address, and adding a new practitioner to an existing address, you must indicate either YES or NO for each practitioner at a location. If a practitioner accepts appointments at a location at least one day per week on a regular basis, then the response is “YES”; otherwise, the response is “NO.”
The “Accepts Appointments?” responses can be viewed once established and modified through the Edit function:
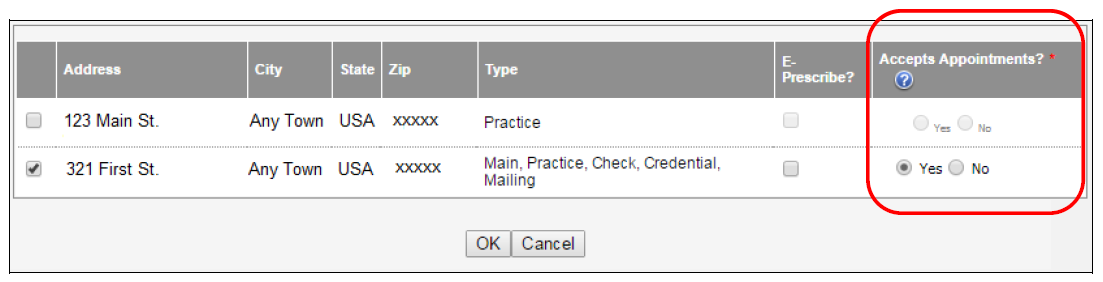
Practices must also confirm the “Accepts Appointments?” answers are accurate when submitting any of these location-related changes. The changes cannot be saved until this statement is confirmed.
Written Notification Required for Mergers and Acquisitions
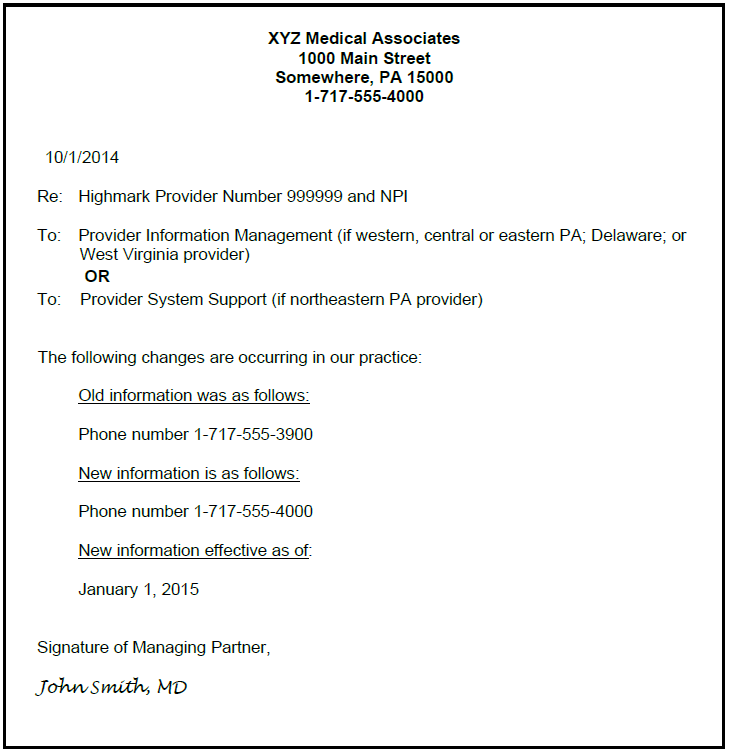
The provider agreement between Highmark and network practitioners is not assignable. In cases of practice mergers, acquisitions, etc., it is necessary to send written notification, on practice letterhead, to Highmark.
For additional information, please see the next section of this unit on Mergers and Acquisitions.
Immediate Notification of Certain Actions
Providers of all types must provide immediate written notification to Highmark in the event of any of the following:
- Termination, suspension, or limitation of license or certification;
- Exclusion, withdrawal, sanctions, or other change in status regarding participation in federal health programs (Medicare, Medicaid, Federal Employee Health Benefit Plan, other programs);
- Change in accreditation status;
- Felony conviction;
- Labor strike or work stoppage; and
- Change in credentialing information.
Notification can be mailed to Provider Information Management at:
| Mail to: | Highmark Blue Shield |
Notification to Highmark
You must send written notification on your practice letterhead of anticipated mergers, acquisitions, etc., at least 45 days, if not sooner as required by your network participation agreement, before the change(s) occur. The managing partner of the practice must sign the written notification. Include the following information:
- Effective date of the change
- Highmark provider number, NPI, new tax identification number* (if applicable)
- Changes to physician staffing
- Changes to physician location
The written notification can be mailed to Highmark:
| Mail to: | Highmark Blue Shield |
New assignment account paperwork will need to be completed – please use the Request for Assignment Account form. The form can also be found on the Provider Resource Center under Resources & Education, then Forms, and then Provider Information Management Forms.
*When reporting a new tax identification number, include the Internal Revenue Service (IRS) Tax Notification as evidence.
Consequences to Not Giving Notice
Most changes will require Highmark to revise existing provider files. In most cases, membership or claims payment will be affected by major changes in your practice. Therefore, if you do not give advance notification, we cannot guarantee accurate membership information and/or claims payments.
Sample Change Notification
If sending written notification on your practice letterhead, please include information in your letter as shown below:
To resign from participation in Highmark’s credentialed network(s) in all service areas, fill out the electronic Request to Terminate a Contracted Network form. This form can also be accessed on the Provider Resource Center – select Resources & Education, then Forms, and then Provider Information Management Forms.
A resignation may be submitted at any time and is effective in accordance with the termination provision in the agreement the provider has executed. A letter will be sent to you advising of the effective date of your resignation.
IMPORTANT: If you decide to resign from the Highmark network(s) by submitting the form above, the resignation will trigger automatic letters to Highmark members, who are your patients, via U.S. Mail, notifying them you have terminated and are no longer in network. Please take this into account before completing the electronic form.
A network provider who engages in practices inconsistent with reasonable standards of care or professional conduct or who does not comply with Highmark contractual or administrative requirements may be subject to corrective action.
Determining Need for Corrective Action
Certain circumstances, acts, or omissions of a professional network provider may result in a requirement that the provider engage in a corrective action or a series of corrective actions to continue participation in the network.
Treatments, procedures, and services that are subject to corrective action include any treatments, procedures, or services that indicate a professional provider is practicing in a manner that is not consistent with reasonable standards of care (including, when applicable, accepted standards of medical care) and service, ethical expectations, contractual obligations, or the administrative requirements of the plan.
Examples of such circumstances, acts, or omissions which may be subject to corrective action include, but are not limited to, the following:
- Clinical quality of care
- Administrative non-compliance
- Unacceptable resource utilization
- Service-related issue
Providers identified with one of these issues will be reported to a Highmark Medical Director. The determination to take corrective action shall be made by a Medical Director.
Determining Need for Corrective Action
For New York providers, a corrective action plan can be initiated by any department or corporate committee. The Health Care Quality Improvement (HCQI) team is responsible to coordinate efforts amongst the Senior Medical Director and appropriate teams that will be integral in the review.
Once Provider Correspondence is reviewed and approved, it is sent out from the HCQI team with instructions, requested materials and a time frame when it is due back.
Forms of Corrective Action
Corrective action may vary according to the situation and may include, but is not limited to, one or more of the following actions as they relate to the circumstance, action, or omission that requires corrective action:
- Sending a written warning to the provider
- Engaging in a discussion or a series of discussions with the provider
- Monitoring the provider’s performance
- Expedited recredentialing
- Requiring that the provider complete a continuing medical education course regarding the treatment, procedure, or service in question
- Limiting the provider’s authority to perform certain procedures
- Requiring that the provider enter a preceptor relationship with another provider
- Monitoring and observing the provider subject to corrective action
- Termination or suspension
Highmark may immediately suspend the network participation status or restrict the clinical privileges of a provider who, in the opinion of the medical director, is engaged in conduct or is practicing in a manner that appears to pose a significant risk or imminent danger to the health, welfare, or safety of a patient or other individual. In such cases, Highmark will investigate the circumstances on an expedited basis.
If the suspension or restriction will last longer than 14 days, the provider will be notified that he/she can request a hearing. The request must be made in writing within 30 days of receipt of the notification.
Corrective Action on Clinical Quality of Care Issues
The determination to take corrective action on a clinical quality of care issue shall be based on an assessment of the severity level of the action based on the judgment of a Highmark Medical Director. The following are general guidelines used by the Medical Directors when assigning severity levels:
|
Severity Level |
Guideline |
|---|---|
|
Minor – low |
Deviation from the standard of care without harm to the member. |
|
Moderate – medium |
Deviation from the standard of care with temporary harm to the member. |
|
Severe – high |
Deviation from the standard of care with harm to the member resulting in permanent sequelae or death. |
Sanctioning
Sanctioning of a provider will occur whenever an assessment of the severity level of action is moderate or severe, and/or the corrective action was a result of an administrative non-compliance circumstance, act, or omission. Sanctioning may result in a provider’s practice not being eligible for participation in certain programs.
Corrective Action Appeals
An appeal shall be made available to a professional network provider before the Highmark Network Quality and Credentials Committee (NQCC), if the practitioner is placed under corrective action.
If an appeal is available, the procedure will be as follows:
|
Step |
Action |
|---|---|
|
1 |
The provider will be given written notice of the proposed action including: (a) the action that has been proposed to be taken against the provider; (b) the reason(s) for the action; (c) that the provider may request an appeal on the proposed action; (d) that the practitioner may participate via phone or in person; and (e) that the provider will waive any appeal rights if an appeal is not requested within 30 days of receipt of the notice of the action. |
|
2 |
If the provider requests an appeal on a timely basis, Highmark will notify the provider of the time and date of the NQCC meeting. |
|
3 |
The appeal shall be held before the NQCC, which is comprised of network practicing providers who will review the information presented and render a decision. The members of the NQCC shall not be in direct economic competition with the provider. |
|
4 |
After completion of the appeal, the provider has the right to receive the written decision of the Credentials Committee from the Medical Director, including a statement of the basis for the decision. The decision of the Credentials Committee is not subject to further appeal. |
Corrective Action Appeals
Corrective Action is discussed with the Senior Medical Director and team who were responsible for the review prior to notification to the provider.
Any Corporate Credential Committee initiated requests for Corrective Action would be determined by the Senior Medical Director and team prior to being discussed with the NY Corporate Committee team for re-credential consideration.
If the provider requests an appeal on a timely basis, Highmark will notify the provider of the time and date of the appeal meeting.
The following entities, which serve the noted regions, are independent licensees of the Blue Cross Blue Shield Association: Western and Northeastern PA: Highmark Inc. d/b/a Highmark Blue Cross Blue Shield, Highmark Choice Company, Highmark Health Insurance Company, Highmark Coverage Advantage Inc., Highmark Benefits Group Inc., First Priority Health, First Priority Life, Highmark Care Benefits Inc., or Highmark Senior Health Company. Central and Southeastern PA: Highmark Inc. d/b/a Highmark Blue Shield, Highmark Benefits Group Inc., Highmark Health Insurance Company, Highmark Choice Company or Highmark Senior Health Company. Delaware: Highmark BCBSD Inc. d/b/a Highmark Blue Cross Blue Shield. West Virginia: Highmark West Virginia Inc. d/b/a Highmark Blue Cross Blue Shield, Highmark Health Insurance Company or Highmark Senior Solutions Company. Western NY: Highmark Western and Northeastern New York Inc. d/b/a Highmark Blue Cross Blue Shield. Northeastern NY: Highmark Western and Northeastern New York Inc. d/b/a Highmark Blue Shield.
All references to “Highmark” in this document are references to the Highmark company that is providing the member’s health benefits or health benefit administration and/or to one or more of its affiliated Blue companies.
All revisions to this Highmark Provider Manual (the “manual” or “Highmark Provider Manual”) are controlled electronically. All paper copies and screen prints are considered uncontrolled and should not be relied upon for any purpose.