Gold Carding Program
Last Updated: Thursday, November 13, 2025
- wv
The information on this page is applicable to providers in Delaware, New York, and Pennsylvania. The Gold Card program in West Virginia is regulated by a state mandate. For information specific to the West Virginia Gold Card program, please see the Highmark Provider Manual Chapter 5, Unit 2.
Clinician Roster
To view a current master list of Gold Carded clinicians, click the link below.
Eligible CPT Codes – Gold Card-eligible procedures and codes are identified in the prior authorization list for your region:
- wpa/ nepa
- cpa/ sepa
- de
Value of Gold Carding
According to the March 2023 American Medical Association (AMA) physician survey, patients and clinicians are frustrated by the delays in care due to the current utilization management process. The Gold Card program provides expedited prior authorization for clinicians who demonstrate adherence to appropriate clinical criteria.
The following is the link to access the March 2023 AMA physician survey:
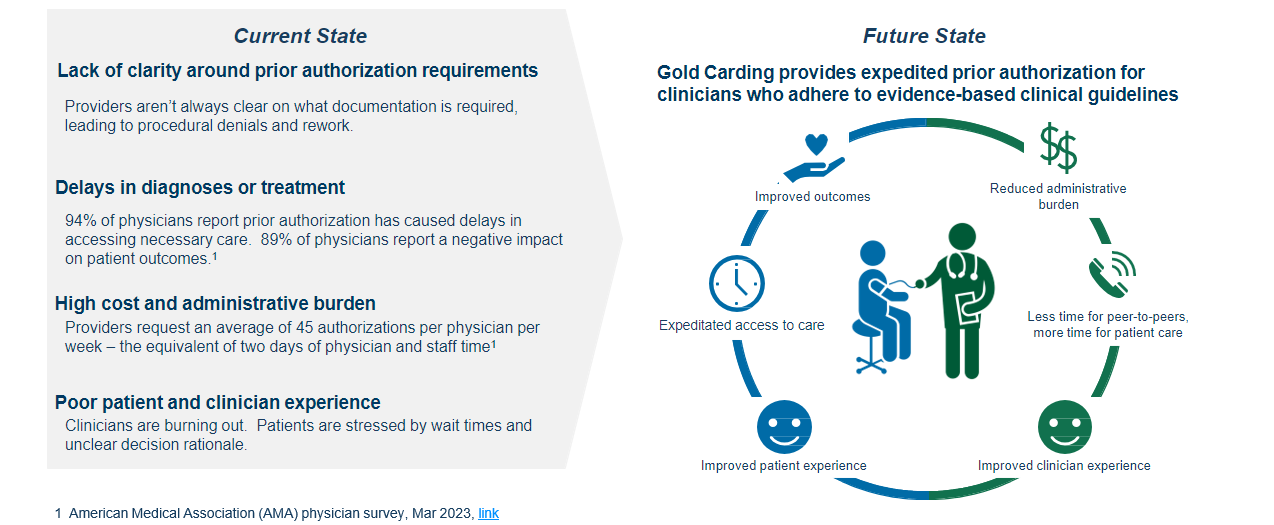
Across the industry, the current state of utilization review and management is too often a barrier to good health. While prior authorizations are intended to ensure compliance with evidence-based practices, they can be an obstacle to appropriate care, delaying diagnosis and treatment.
The following is a link to a September 2024 Highmark Health Digital Magazine article:
Program Overview
Eligibility*
- Individual clinicians with a minimum submission history of three* cases per gold carded modality are eligible.
- Individual clinicians must have a 99%* or higher approval rating for the specified gold carded Current Procedural Terminology (CPT) codes and modalities.
- Plans must be one of the following: Commercial, Affordable Care Act, Medicare Advantage.
- Pre-notification must be submitted per the details below. Pre-notifications can be submitted using the same process as a normal authorization request via the Availity Essentials provider portal.
*Eligibility criteria can vary in accordance with state mandates.
Enrollment
- Highmark automatically enrolls clinicians bi-annually, when eligibility criteria are met.
- Highmark sends out communication to the qualifying clinician practice when auto-enrolled in the program.
Management
- Once the clinician is Gold Carded, Highmark monitors ordering trends.
- Highmark conducts random auditing and/or targeted auditing based on program enrollment and utilization variances.
Frequently Asked Questions
Gold Card Pre-notification Process
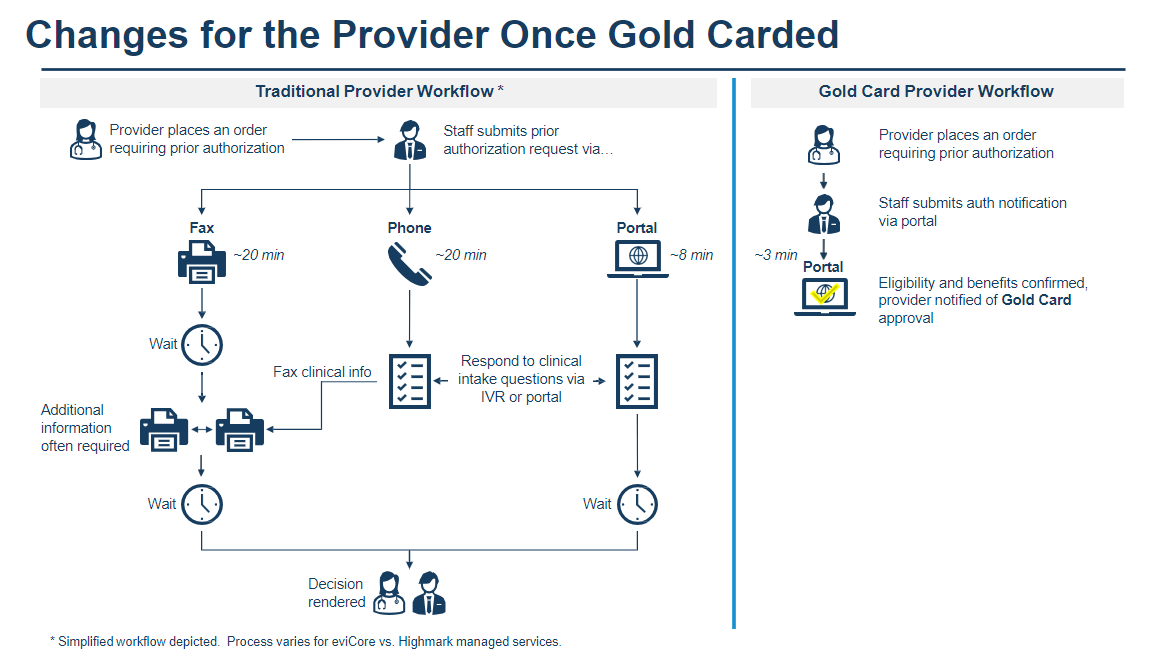
Providers will follow a simplified pre-notification process once they are Gold Carded:
- Log into the Availity Essentials provider portal.
- Submit the pre-notification following the same process as beginning an authorization request.
- The following information should be included when submitting the pre-notification:
- Member ID, name, and date of birth
- Procedure, ordering provider, place of service, primary diagnosis code
- Person submitting the information and phone number
- Performing provider if available
- The system will recognize the provider and CPT code as meeting Gold Card program criteria.
- No clinical information is needed.
- Approval is granted immediately without additional review.
- A pre-notification must be submitted for claims to pay regardless of Gold Card program status.
- For additional questions or to report an issue, please email goldcardinquiries@highmark.com.